Userid: CPM Schema: instrx Leadpct: 100% Pt. size: 9
Draft Ok to Print
AH XSL/XML
Fileid: … 094c&1095c/2023/a/xml/cycle04/source (Init. & Date) _______
Page 1 of 18 9:16 - 26-Sep-2023
The type and rule above prints on all proofs including departmental reproduction proofs. MUST be removed before printing.
2023
Instructions for Forms
1094-C and 1095-C
Department of the Treasury
Internal Revenue Service
Section references are to the Internal Revenue Code unless
otherwise noted.
Future Developments
For the latest information about developments related to Form
1094-C, Transmittal of Employer-Provided Health Insurance
Offer and Coverage Information Returns, and Form 1095-C,
Employer-Provided Health Insurance Offer and Coverage, and
the instructions, such as legislation enacted after they were
published, go to
IRS.gov/Form1094C and IRS.gov/Form1095C.
What’s New
The electronic-filing threshold for information returns required to
be filed on or after January 1, 2024, has been decreased to 10 or
more returns. See Electronic Filing, later.
Additional Information
For information related to the Affordable Care Act, visit IRS.gov/
ACA. For the final regulations under section 6056, Information
Reporting by Applicable Large Employers on Health Insurance
Coverage Offered Under Employer-Sponsored Plans, see T.D.
9661, 2014-13 I.R.B. 855, at
IRS.gov/irb/2014-13_IRB/ar09.html.
For the final regulations under section 6055, Information
Reporting of Minimum Essential Coverage, see T.D. 9660,
2014-13 I.R.B. 842, at IRS.gov/irb/2014-13_IRB/ar08.html and
T.D. 9970, 2023-02 I.R.B. 311, at IRS.gov/irb/2023-02_IRB. For
the final regulations under section 4980H, Shared Responsibility
for Employers Regarding Health Coverage, see T.D. 9655,
2014-9 I.R.B. 541, at
IRS.gov/irb/2014-9_IRB/ar05.html. For
answers to frequently asked questions regarding the employer
shared responsibility provisions and related information reporting
requirements, visit IRS.gov.
For information related to filing Forms 1094-C and 1095-C
electronically, visit IRS.gov/AIR. For FAQs specifically related to
completing Forms 1094-C and 1095-C, go to IRS.gov/
Affordable-Care-Act/Employers/Questions-and-Answers-about-
Information-Reporting-by-Employers-on-Form-1094-C-and-
Form-1095-C.
For additional guidance and proposed regulatory changes
relating to section 6055, including the requirement to solicit the
TIN of each covered individual for purposes of the reporting of
health coverage information, see Proposed Regulations section
1.6055-1(h) and Regulations section 301.6724-1.
General Instructions for
Forms 1094-C and 1095-C
See Definitions, later, for key terms used in these instructions.
Purpose of Form
Employers with 50 or more full-time employees (including
full-time equivalent employees) in the previous year use Forms
1094-C and 1095-C to report the information required under
sections 6055 and 6056 about offers of health coverage and
enrollment in health coverage for their employees. Form 1094-C
must be used to report to the IRS summary information for each
Applicable Large Employer (ALE Member) (defined below) and
to transmit Forms 1095-C to the IRS. Form 1095-C is used to
report information about each employee to the IRS and to the
employee. Forms 1094-C and 1095-C are used in determining
whether an ALE Member owes a payment under the employer
shared responsibility provisions under section 4980H. Form
1095-C is also used in determining the eligibility of employees
for the premium tax credit.
ALE Members that offer employer-sponsored, self-insured
coverage also use Form 1095-C to report information to the IRS
and to employees about individuals who have minimum essential
coverage under the employer plan.
Who Must File
An ALE Member must file one or more Forms 1094-C (including
a Form 1094-C designated as the Authoritative Transmittal,
whether or not filing multiple Forms 1094-C), and must file a
Form 1095-C for each employee who was a full-time employee
of the ALE Member for any month of the calendar year.
Generally, the ALE Member is required to furnish a copy of the
Form 1095-C (or a substitute form) to the employee.
An ALE Member is, generally, a single person or entity that is
an Applicable Large Employer, or if applicable, each person or
entity that is a member of an Aggregated ALE Group. An
Applicable Large Employer, generally, is an employer with 50 or
more full-time employees (including full-time equivalent
employees) in the previous year. For purposes of determining if
an employer or group of employers is an Applicable Large
Employer, all ALE Members under common control (an
Aggregated ALE Group) are aggregated together. If the
Aggregated ALE Group, taking into account the employees of all
ALE Members in the group, employed on average 50 or more
full-time employees (including full-time equivalent employees) on
business days during the preceding calendar year, then the
Aggregated ALE Group is an Applicable Large Employer and
each separate employer within the group is an ALE Member.
Each ALE Member is required to file Forms 1094-C and 1095-C
reporting offers of coverage to its full-time employees (even if the
ALE Member has fewer than 50 full-time employees of its own).
For more information on which employers are subject to the
employer shared responsibility provisions of section 4980H, see
Employer in the Definitions section of these instructions. For
more information on determining full-time employees, see
Full-Time Employee in the Definitions section of these
instructions, which includes information on the treatment of new
hires and employees in Limited Non-Assessment Periods.
For purposes of reporting on Forms 1094-C and 1095-C,
an employee in a Limited Non-Assessment Period is not
considered a full-time employee during that period.
Reporting by Employers That
Sponsor Self-Insured Health Plans
An employer that offers health coverage through a self-insured
health plan must report information about each individual
enrolled in such coverage. For an employer that is an ALE
Member, this information must be reported on Form 1095-C, Part
III, for any employee who is enrolled in coverage (and any
spouse or dependent of that employee). See the option to file
TIP
Sep 26, 2023
Cat. No. 63018M
Page 2 of 18 Fileid: … 094c&1095c/2023/a/xml/cycle04/source 9:16 - 26-Sep-2023
The type and rule above prints on all proofs including departmental reproduction proofs. MUST be removed before printing.
Form 1094-B and Form 1095-B, rather than Form 1094-C and
Form 1095-C, to report coverage of certain non-employees,
below.
ALE Members that offer health coverage through an
employer-sponsored, self-insured health plan must complete
Form 1095-C, Parts I, II, and III, for any employee who enrolls in
the health coverage, whether or not the employee is a full-time
employee for any month of the calendar year.
For full-time employees enrolled in an ALE Member’s
self-insured coverage, including an employee who was a
full-time employee for at least 1 month of the calendar year, the
ALE Member must complete Form 1095-C, Part II, according to
the generally applicable instructions, and should not enter code
1G on line 14 for any month. For an employee enrolled in an ALE
Member’s self-insured coverage who is not a full-time employee
for any month of the calendar year (meaning that for all 12
calendar months the employee was not a full-time employee), for
Form 1095-C, Part II, the ALE Member must enter code 1G on
line 14 in the “All 12 Months” column or in the separate monthly
boxes for all 12 calendar months, and the ALE Member need not
complete Part II, lines 15 and 16.
An individual coverage HRA is a self-insured group
health plan and is therefore an eligible
employer-sponsored plan. An individual is ineligible for a
premium tax credit (PTC) for a month if the individual is covered
by an individual coverage HRA or eligible for an individual
coverage HRA that is affordable.
An employer that offers employer-sponsored, self-insured
health coverage but is not an ALE Member should not file Forms
1094-C and 1095-C, but should instead file Forms 1094-B and
1095-B to report information for employees who enrolled in the
employer-sponsored, self-insured health coverage.
Note. If an ALE Member is offering health coverage to
employees other than under a self-insured plan, such as through
an insured health plan or a multiemployer health plan, the issuer
of the insurance or the sponsor of the plan providing the
coverage is required to furnish the information about their health
coverage to any enrolled employees, and the ALE Member
should not complete Form 1095-C, Part III, for those employees.
Reporting of Enrollment Information
for Non-Employees: Option
To Use Forms 1094-B and 1095-B
ALE Members that offer employer-sponsored, self-insured
health coverage to non-employees who enroll in the coverage
may use Forms 1094-B and 1095-B, rather than Form 1095-C,
Part III, to report coverage for those individuals and other family
members. For this purpose, a non-employee includes, for
example, a non-employee director, an individual who was a
retired employee during the entire year, or a non-employee
COBRA beneficiary, including a former employee who
terminated employment during a previous year.
For information on reporting for non-employees enrolled in an
employer-sponsored, self-insured health plan using Forms
1094-B and 1095-B, see the instructions for those forms.
For ALE Members that choose to use Form 1095-C to report
coverage information for non-employees enrolled in an
employer-sponsored, self-insured health plan, see the specific
instructions for Form 1095-C, Part III—Covered Individuals
(Lines 18–30), later. Form 1095-C may be used only if the
individual identified on line 1 has an SSN.
TIP
Substitute Statements to Recipients
If you are not using the official IRS form to furnish statements to
recipients, see Pub. 5223, General Rules and Specifications for
Affordable Care Act Substitute Forms 1095-A, 1094-B, 1095-B,
1094-C, and 1095-C, which explains the requirements for format
and content of substitute statements to recipients. You may
develop them yourself or buy them from a private printer.
Substitute statements furnished to recipients may be in portrait
format; however, substitute returns filed with the IRS using paper
must be printed in landscape format.
Authoritative Transmittal for ALE
Members Filing Multiple Forms 1094-C
A Form 1094-C must be filed when an ALE Member files one or
more Forms 1095-C. An ALE Member may choose to file
multiple Forms 1094-C, each accompanied by Forms 1095-C for
a portion of its employees, provided that a Form 1095-C is filed
for each employee for whom the ALE Member is required to file.
If an ALE Member files more than one Form 1094-C, one (and
only one) Form 1094-C filed by the ALE Member must be
identified on line 19, Part I, as the Authoritative Transmittal, and,
on the Authoritative Transmittal, the ALE Member must report
certain aggregate data for all full-time employees and all
employees, as applicable, of the ALE Member.
Example 1. Employer A, an ALE Member, files a single Form
1094-C, attaching Forms 1095-C for each of its 100 full-time
employees. This Form 1094-C should be identified as the
Authoritative Transmittal on line 19, and the remainder of the
form completed as indicated in the instructions for
line 19, later.
Example 2. Employer B, an ALE Member, files two Forms
1094-C, one for each of its two operating divisions, Division X
and Division Y. (Division X and Division Y are units of the same
ALE Member, and thus both report under the same employer
identification number (EIN); they are not members of an
Aggregated ALE Group.) Attached to one Form 1094-C are
Forms 1095-C for the 200 full-time employees of Division X, and
attached to the other Form 1094-C are Forms 1095-C for the
1,000 full-time employees of Division Y. One of these Forms
1094-C should be identified as the Authoritative Transmittal on
line 19, and should include aggregate employer-level data for all
1,200 full-time employees of Employer B as well as the total
number of employees of Employer B, as applicable, as required
in Parts II, III, and IV of Form 1094-C. The other Form 1094-C
should not be identified as the Authoritative Transmittal on
line 19, and should report on line 18 only the number of Forms
1095-C that are attached to that Form 1094-C, and should leave
the remaining sections of the form blank, as indicated in the
instructions for
line 19, later.
Note. Each ALE Member must file its own Forms 1094-C and
1095-C under its own separate EIN, even if the ALE Member is
part of an Aggregated ALE Group. No Authoritative Transmittal
should be filed for an Aggregated ALE Group.
Example 3. Assume that Employer A from Example 1 is a
member of the same Aggregated ALE Group as Employer B
from
Example 2. Accordingly, Employer A and Employer B are
separate ALE Members filing under separate EINs. Forms
1094-C should be filed in the same manner indicated in
Examples 1 and 2. Employer A should include only information
about employees of Employer A in its Authoritative Transmittal,
and Employer B should include only information about
employees of Employer B in its Authoritative Transmittal. No
Authoritative Transmittal should be filed for the Aggregated ALE
Group reporting combined data for employees of both Employer
A and Employer B.
Similar rules apply for a Governmental Unit that has
delegated its reporting responsibilities for some of its employees
-2-
Instructions for Forms 1094-C and 1095-C (2023)
Page 3 of 18 Fileid: … 094c&1095c/2023/a/xml/cycle04/source 9:16 - 26-Sep-2023
The type and rule above prints on all proofs including departmental reproduction proofs. MUST be removed before printing.
to another Governmental Unit—see Designated Governmental
Entity (DGE) in the Definitions section of these instructions for
more information. In the case of a Governmental Unit that has
delegated its reporting responsibilities for some of its employees,
the Governmental Unit must ensure that among the multiple
Forms 1094-C filed by or on behalf of the Governmental Unit
transmitting Forms 1095-C for the Governmental Unit’s
employees, one of the filed Forms 1094-C is designated as the
Authoritative Transmittal and reports aggregate employer-level
data for the Governmental Unit, as required in Parts II, III, and IV
of Form 1094-C.
Example. County is an Aggregated ALE Group made up of
the ALE Members School District, the Police District, and the
County General Office. The School District designates the state
to report on behalf of the teachers and reports for itself for its
remaining full-time employees. In this case, either the School
District or the state must file an Authoritative Transmittal
reporting aggregate employer-level data for the School District.
One Form 1095-C for Each
Employee of ALE Member
For each full-time employee of an ALE Member, there must be
only one Form 1095-C filed for employment with that ALE
Member. For example, if an ALE Member separately reports for
each of its two divisions, the ALE Member must combine the
offer and coverage information for any employee who worked at
both divisions during the calendar year so that a single Form
1095-C is filed for the calendar year for that employee, which
reports information for all 12 months of the calendar year from
that ALE Member.
In contrast, a full-time employee who works for more than one
ALE Member that is a member of the same Aggregated ALE
Group must receive a separate Form 1095-C from each ALE
Member. For any calendar month in which a full-time employee
works for more than one ALE Member of an Aggregated ALE
Group, only one ALE Member is treated as the employer of that
employee for reporting purposes (generally, the ALE Member for
whom the employee worked the greatest number of hours of
service), and only that ALE Member reports for that employee for
that calendar month. The other ALE Member is not required to
report for that employee for that calendar month, unless the
other ALE Member is otherwise required to file Form 1095-C for
that employee because the individual was a full-time employee
of that ALE Member for a different month of the same calendar
year. In this case, the individual may be treated as not employed
by that ALE Member for that calendar month. If under these
rules, an ALE Member is not required to report for an employee
for any month in the calendar year, the ALE Member is not
required to report for that full-time employee for that calendar
year. For a description of the rules related to determining which
ALE Member in an Aggregated ALE Group is treated as the
employer for a month in this situation, see the definition of
Employee.
Example. Employer A and Employer B are separate ALE
Members that belong to the same Aggregated ALE Group. Both
Employer A and Employer B offer coverage through the AB
health plan, which is an insured plan. In January and February,
Employee has 130 hours of service for Employer A and no hours
of service for Employer B. In March, Employee has 100 hours of
service for Employer A and 30 hours of service for Employer B.
In April through December, Employee has 130 hours of service
for Employer B and no hours of service for Employer A.
Employer A is the employer of Employee for filing purposes for
January, February, and March. Employer A should file Form
1095-C for Employee reporting offers of coverage using the
appropriate code on line 14 for January, February, and March;
should complete lines 15 and 16 per the instructions; and should
include Employee in the count of total employees and full-time
employees reported for those months on Form 1094-C. For the
months April through December, on Form 1095-C, Employer A
should enter code 1H (no offer of coverage) on line 14, leave
line 15 blank, and enter code 2A (not an employee) on line 16
(since Employee is treated as an employee of Employer B and
not as an employee of Employer A in those months), and should
exclude Employee from the count of total employees and
full-time employees reported for those months on Form 1094-C.
When To File
You will meet the requirement to file Forms 1094-C and 1095-C if
the forms are properly addressed and mailed on or before the
due date. If the due date falls on a weekend or legal holiday, then
the due date is the following business day. A business day is any
day that is not a Saturday, Sunday, or legal holiday.
Generally, you must file Forms 1094-C and 1095-C by
February 28 if filing on paper (or March 31 if filing electronically)
of the year following the calendar year to which the return
relates. For calendar year 2023, Forms 1094-C and 1095-C are
required to be filed by February 28, 2024, or April 1, 2024, if filing
electronically.
See Furnishing Forms 1095-C to Employees for information
on when Form 1095-C must be furnished.
Extensions
You can get an automatic 30-day extension of time to file by
completing Form 8809, Application for Extension of Time To File
Information Returns. The form may be submitted on paper, or
through the FIRE System either as a fill-in form or an electronic
file. No signature or explanation is required for the extension.
However, you must file Form 8809 on or before the due date of
the returns in order to get the 30-day extension. Under certain
hardship conditions, you may apply for an additional 30-day
extension. See the Instructions for Form 8809 for more
information.
How to apply. File Form 8809 as soon as you know that a
30-day extension of time to file is needed. See the instructions
for Form 8809. Mail or fax Form 8809 using the address and
phone number listed in the instructions. You can also submit the
extension request online through the FIRE System. You are
encouraged to submit requests using the online fill-in form. See
Pub. 1220 for more information on filing online or electronically.
Where To File
Send all information returns filed on paper to the following:
If your principal business,
office or agency, or legal
residence, in the case of an
individual, is located in:
Use the following address:
▼ ▼
Alabama, Arizona, Arkansas,
Connecticut, Delaware, Florida,
Georgia, Kentucky, Louisiana,
Maine, Massachusetts,
Mississippi, New Hampshire,
New Jersey, New Mexico, New
York, North Carolina, Ohio,
Pennsylvania, Rhode Island,
Texas, Vermont, Virginia,
West Virginia
Department of the Treasury
Internal Revenue Service
Center
Austin, TX 73301
Instructions for Forms 1094-C and 1095-C (2023)
-3-
Page 4 of 18 Fileid: … 094c&1095c/2023/a/xml/cycle04/source 9:16 - 26-Sep-2023
The type and rule above prints on all proofs including departmental reproduction proofs. MUST be removed before printing.
If your principal business,
office or agency, or legal
residence, in the case of an
individual, is located in:
Use the following address:
▼ ▼
Alaska, California, Colorado,
District of Columbia, Hawaii,
Idaho, Illinois, Indiana, Iowa,
Kansas, Maryland, Michigan,
Minnesota, Missouri, Montana,
Nebraska, Nevada, North
Dakota, Oklahoma, Oregon,
South Carolina, South Dakota,
Tennessee, Utah, Washington,
Wisconsin, Wyoming
Department of the Treasury
Internal Revenue Service
Center
P.O. Box 219256
Kansas City, MO 64121-9256
If your legal residence or principal place of business or
principal office or agency is outside the United States, file with
the Department of the Treasury, Internal Revenue Service
Center, Austin, TX 73301.
Shipping and mailing. If you are filing on paper, send the
forms to the IRS in a flat mailing (not folded), and do not
paperclip or staple the forms together. If you are sending many
forms, you may send them in conveniently sized packages. On
each package, write your name, number the packages
consecutively, and place Form 1094-C in package number one.
Postal regulations require forms and packages to be sent by
First-Class Mail. Returns filed with the IRS must be printed in
landscape format.
Keeping copies. Generally, keep copies of information returns
you filed with the IRS or have the ability to reconstruct the data
for at least 3 years, from the due date of the returns.
Electronic Filing
If you are required to file 10 or more
information returns during the year, you
must file the forms electronically. The
10-or-more requirement applies in the aggregate to certain
information returns that are original or corrected returns.
Accordingly, a filer may be required to file fewer than 10 Forms
1094-C and 1095-C, but still have an electronic filing obligation
based on other kinds of information returns filed. The electronic
filing requirement does not apply if you request and receive a
hardship waiver. The IRS encourages you to file electronically
even though you are filing fewer than 10 returns.
Waiver. To receive a waiver from the required filing of
information returns electronically, submit Form 8508. You are
encouraged to file Form 8508 at least 45 days before the due
date of the returns, but no later than the due date of the return.
The IRS does not process waiver requests until January 1 of the
calendar year the returns are due. You cannot apply for a waiver
for more than 1 tax year at a time. If you need a waiver for more
than 1 tax year, you must reapply at the appropriate time each
year. If a waiver for original returns is approved, any corrections
for the same types of returns will be covered under the waiver.
However, if you submit original returns electronically but you
want to submit your corrections on paper, a waiver must be
approved for the corrections if you must file 10 or more
corrections. If you receive an approved waiver, do not send a
copy of it to the service center where you file your paper returns.
Keep the waiver for your records only.
If you are required to file electronically but fail to do so, and
you do not have an approved waiver, you may be subject to a
penalty of $310 per return for failure to file electronically unless
you establish reasonable cause. However, you can file up to 10
returns on paper; those returns will not be subject to a penalty for
failure to file electronically. The penalty applies separately to
original returns and corrected returns.
Pub. 5165, Guide for Electronically Filing Affordable Care Act
(ACA) Information Returns for Software Developers and
Transmitters, specifies the communication procedures,
transmission formats, business rules, and validation procedures,
and explains when a return will be accepted, accepted with
errors, or rejected, for returns filed electronically for calendar
year 2023 through the ACA Information Return (AIR) system. To
develop software for use with the AIR system, software
developers, transmitters, and issuers, including ALE Members
filing their own Forms 1094-C and 1095-C, should use the
guidelines provided in Pub. 5165 along with the Extensible
Markup Language (XML) Schemas published on IRS.gov.
Reminder. The formatting directions in these instructions (for
example, the directions to enter the 9-digit EIN, including the
dash on line 2 of Form 1094-C) are for the preparation of paper
returns. When filing forms electronically, the formatting set forth
in the XML Schemas and Business Rules published on IRS.gov
must be followed rather than the formatting directions in these
instructions. For more information regarding electronic filing, see
Pubs. 5164 and 5165.
Substitute Returns Filed With the IRS
If you are filing your returns on paper, see Pub. 5223 for
specifications for private printing of substitute information
returns. You may not request special consideration. Only forms
that conform to the official form and the specifications in Pub.
5223 are acceptable for filing with the IRS. Substitute returns
filed with the IRS must be printed in landscape format.
VOID Box
Do not use this box on Form 1095-C.
Corrected Forms 1094-C and 1095-C
For information about filing corrections electronically, see
section 7.1 of Pub. 5165.
Corrected Returns
A corrected return should be filed as soon as possible after an
error is discovered. File the corrected returns as follows.
Form 1094-C. If correcting information on the Authoritative
Transmittal (identified on Part I, line 19, as the Authoritative
Transmittal, one (and only one) of which must be filed for each
ALE Member reporting aggregate employer-level data for all
full-time employees and employees of the ALE Member), file a
standalone, fully completed Form 1094-C, including the correct
information, and enter an “X” in the “CORRECTED” checkbox.
Do not file a return correcting information on a Form 1094-C that
is not the Authoritative Transmittal.
Do not file any other documents (for example, Form
1095-C) with the corrected Authoritative Transmittal.
Form 1095-C. If correcting information on a Form 1095-C that
was previously filed with the IRS, file a fully completed Form
1095-C, including the correct information and enter an “X” in the
“CORRECTED” checkbox. File a Form 1094-C (
do not mark the
“CORRECTED” checkbox on Form 1094-C) with corrected
Form(s) 1095-C. Furnish the employee a copy of the corrected
Form 1095-C, unless the ALE Member was, and continues to be,
eligible for and used the alternative method of furnishing under
the Qualifying Offer Method for that employee for that year’s
furnishing. For more information, see Alternative method of
TIP
CAUTION
!
-4-
Instructions for Forms 1094-C and 1095-C (2023)
Page 5 of 18 Fileid: … 094c&1095c/2023/a/xml/cycle04/source 9:16 - 26-Sep-2023
The type and rule above prints on all proofs including departmental reproduction proofs. MUST be removed before printing.
furnishing Form 1095-C to employees under the Qualifying Offer
Method.
Forms 1095-C filed with incorrect dollar amounts on line 15,
Employee Required Contribution, may fall under a safe harbor
for certain de minimis errors. The safe harbor generally applies if
no single amount in error differs from the correct amount by more
than $100. If the safe harbor applies, you will not have to correct
Form 1095-C to avoid penalties. However, if the recipient elects
for the safe harbor not to apply, you may have to issue a
corrected Form 1095-C to avoid penalties. For more information,
see Notice 2017-9, 2017-4 I.R.B. 542, at
IRS.gov/irb/2017-04
IRB/ar11.html.
Note. Enter an “X” in the “CORRECTED” checkbox only when
correcting a Form 1095-C previously filed with the IRS. If you are
correcting a Form 1095-C that was previously furnished to a
recipient, but not filed with the IRS, write, type, or print
“CORRECTED” on the new Form 1095-C furnished to the
recipient.
Correcting information affecting statement furnished to
employee using an Alternative Furnishing Method under
the Qualifying Offer Method. If an ALE Member eligible to use
the Qualifying Offer Method had furnished the employee an
alternative statement, the ALE Member must furnish the
employee a corrected statement if it filed a corrected Form
1095-C correcting the ALE Member’s name, EIN, address, or
contact name and telephone number. If the ALE Member is no
longer eligible to use an alternative furnishing method for the
employee for whom it filed a corrected Form 1095-C, it must
furnish a Form 1095-C to the employee and advise the employee
that Form 1095-C replaces the statement it had previously
furnished.
If you fail to file correct information returns or fail to
furnish a correct recipient statement, you may be subject
to a penalty. However, you are not required to file
corrected returns for missing or incorrect TINs if you meet the
reasonable cause criteria. For additional information, see Pub.
1586, Reasonable Cause Regulations and Requirements for
Missing and Incorrect Name/TINs on Information Returns.
See the charts for examples of errors and step-by-step
instructions for filing corrected returns.
CAUTION
!
TIP
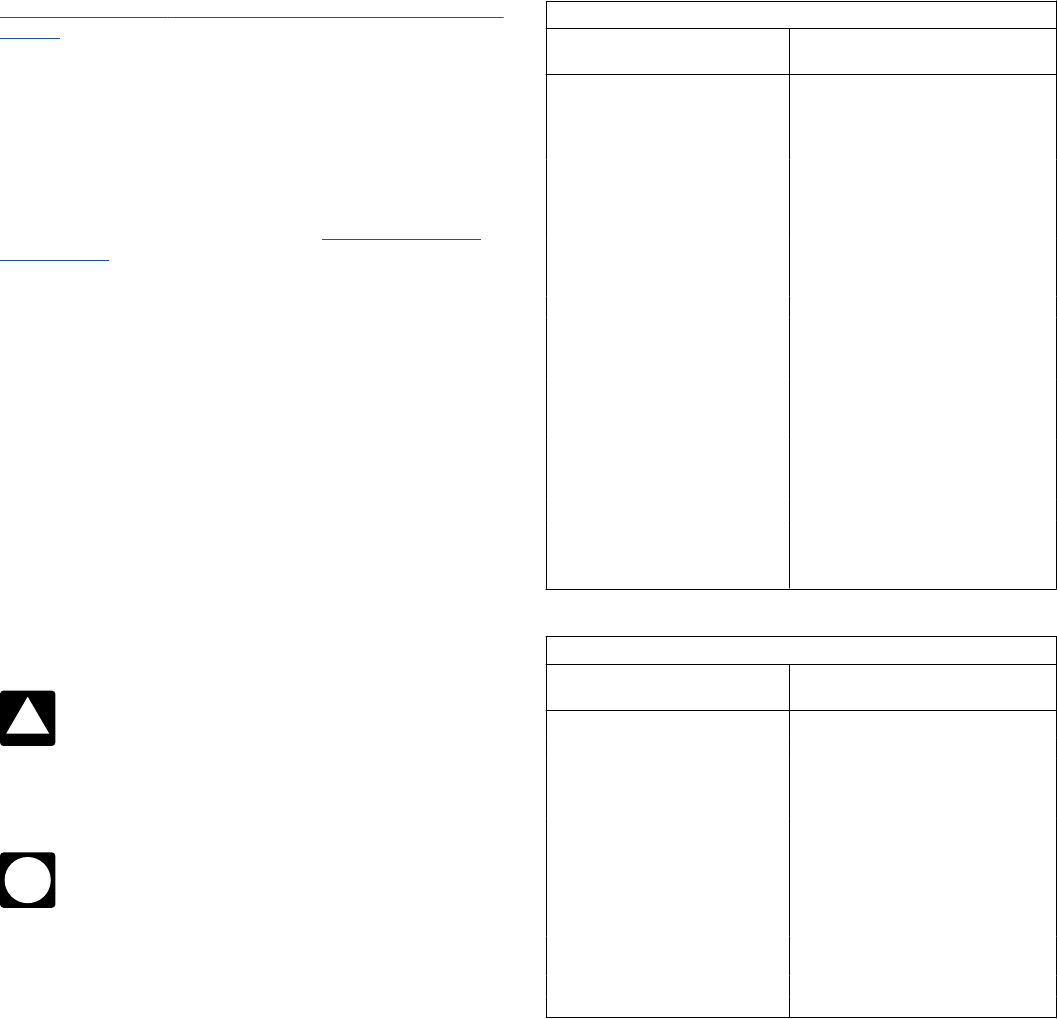
Original Authoritative Transmittal Form 1094-C
IF any of the following are
incorrect ...
THEN ...
ALE Member or Designated
Government Entity (Name and/or
EIN)
1. Prepare a new Authoritative
Transmittal, Form 1094-C.
2. Enter an “X” in the “CORRECTED”
checkbox at the top of the form.
Total number of Forms 1095-C filed
by and/or on behalf of ALE Member
3. Submit the standalone corrected
Form 1094-C with the correct
information present.
Aggregated ALE Group Membership
Certifications of Eligibility
Minimum Essential Coverage Offer
Indicator
Section 4980H Full-Time Employee
Count for ALE Member
Aggregated Group Indicator
Other ALE Members of Aggregated
ALE Group (Name and/or EIN)
Original Form 1095-C Submitted to IRS and Furnished to Employee
IF any of the following are
incorrect ...
THEN ...
Name, SSN, ALE Member EIN 1. Prepare a new Form 1095-C.
Offer of Coverage (line 14) 2. Enter an “X” in the “CORRECTED”
checkbox at the top of the form.
Employee Required Contribution 3. Submit corrected Forms 1095-C with
a non-authoritative Form 1094-C
transmittal to the IRS.
Section 4980H Safe Harbor and
Other Relief Codes (line 16)
4. Furnish a corrected Form 1095-C to
the employee.
Covered Individuals Information
Instructions for Forms 1094-C and 1095-C (2023)
-5-
Page 6 of 18 Fileid: … 094c&1095c/2023/a/xml/cycle04/source 9:16 - 26-Sep-2023
The type and rule above prints on all proofs including departmental reproduction proofs. MUST be removed before printing.
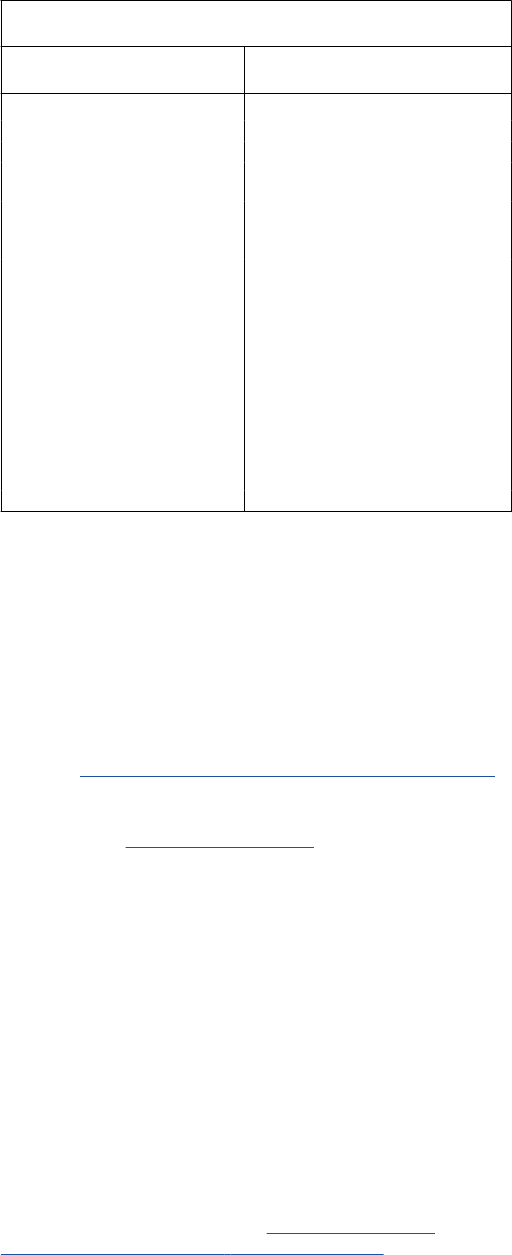
Original Alternative Furnishing Method Under the Qualifying Offer
Method Statement Furnished to Employee
IF any of the following are
incorrect ...
THEN ...
Name, SSN, ALE Member EIN • Submission to the IRS:
1. Prepare a new Form 1095-C.
Offer of Coverage 2. Enter an “X” in the “CORRECTED”
checkbox at the top of the form.
3. Submit corrected Form 1095-Cs
with a non-authoritative Form 1094-C
transmittal to the IRS.
• Furnish to employee:
If, after the correction, the ALE Member
is still eligible to use the alternative
furnishing method under the Qualifying
Offer Method, furnish the employee
either a Form 1095-C or corrected
statement.
If the ALE Member is no longer eligible
to use the alternative furnishing method
with respect to the employee, furnish a
Form 1095-C to the employee.
Furnishing Forms 1095-C to Employees
You will meet the requirement to furnish Form 1095-C to an
employee if the form is properly addressed and mailed on or
before the due date. If the due date falls on a weekend or legal
holiday, then the due date is the following business day. A
business day is any day that is not a Saturday, Sunday, or legal
holiday.
An ALE member must furnish a Form 1095-C to each of its
full-time employees by March 1, 2024, for the 2023 calendar
year. See
Extensions of time to furnish statements to recipients,
below.
For more information on alternative furnishing methods for
employers, see
Qualifying Offer Method, later.
Filers of Form 1095-C may truncate the social security
number (SSN) of an individual (the employee or any family
member of the employee receiving coverage) on Form 1095-C
statements furnished to employees by showing only the last four
digits of the SSN and replacing the first five digits with asterisks
(*) or Xs. Truncation is not allowed on forms filed with the IRS. In
addition, an ALE Member's EIN may not be truncated on the
statements furnished to employees or the forms filed with the
IRS.
Except as provided below, statements must be furnished on
paper by mail (or hand delivered), unless the recipient
affirmatively consents to receive the statement in an electronic
format. If mailed, the statement must be sent to the employee's
last known permanent address, or if no permanent address is
known, to the employee's temporary address. For more
information on furnishing statements to non-full-time employees
and non-employees who are enrolled in employer-sponsored
self-insured health coverage, see
Alternative manner of
furnishing statements to non-full-time employees, later.
Consent to furnish statement electronically. An ALE
Member is required to obtain affirmative consent to furnish a
statement electronically. This requirement ensures that
statements are furnished electronically only to individuals who
are able to access them. The consent must relate specifically to
receiving the Form 1095-C electronically. An individual may
consent on paper or electronically, such as by email. If consent is
on paper, the individual must confirm the consent electronically.
A statement may be furnished electronically by email or by
informing the individual how to access the statement on the ALE
Member’s website. Statements reporting coverage and offers of
coverage under an expatriate health plan, however, may be
furnished electronically unless the recipient explicitly refuses to
consent to receive the statement in an electronic format. Specific
information on consents to furnish statements electronically can
be found in Regulations section 301.6056-2.
Extensions of time to furnish statements to recipients. The
due date for furnishing Form 1095-C is automatically extended
from January 31, 2024, to March 1, 2024. Thus, no additional
extensions will be granted.
Information reporting penalties. All employers subject to the
employer shared responsibility provisions and other employers
that sponsor self-insured group health plans that fail to comply
with the applicable information reporting requirements may be
subject to the general reporting penalty provisions for failure to
file correct information returns and failure to furnish correct
payee statements. For returns required to be made and
statements required to be furnished for 2023 tax year returns, the
following apply.
•
The penalty for failure to file a correct information return is
$310 for each return for which the failure occurs, with the total
penalty for a calendar year not to exceed $3,783,000.
•
The penalty for failure to provide a correct payee statement is
$310 for each statement for which the failure occurs, with the
total penalty for a calendar year not to exceed $3,783,000.
•
Special rules apply that increase the per-statement and total
penalties if there is intentional disregard of the requirement to file
the returns and furnish the required statements.
Penalties may be waived if the failure was due to reasonable
cause and not willful neglect. See section 6724 and Regulations
section 301.6724-1 and Regulations section 1.6055-1(h) (which
relate to Form 1095-C, Part III). For additional information, see
Pub. 1586.
Alternative manner of furnishing statements to
non-full-time employees. If you are an ALE member that offers
employer-sponsored, self-insured health coverage and meets
the requirements of Regulations section 1.6055-1(g), you may
use the alternative manner of furnishing statements to
non-full-time employees and non-employees who are enrolled in
the self-insured health coverage. To use the alternative manner
of furnishing statements, the following conditions must be met.
•
The employer must provide clear and conspicuous notice, in a
location on its website that is reasonably accessible to all
individuals, stating that individuals may receive a copy of their
statement upon request. The notice must include an email
address, a physical address to which a request for a statement
may be sent, and a telephone number that individuals may use
to contact the employer with any questions. A notice posted on
an employer’s website must be written in plain, non-technical
terms and with letters of a font size large enough, including any
visual clues or graphical figures, to call to a viewer’s attention
that the information pertains to tax statements reporting that
individuals had health coverage. For example, an employer’s
website provides a clear and conspicuous notice if it (1) includes
a statement on the main page, or a link on the main page,
reading “Tax Information,” to a secondary page that includes a
statement, in capital letters, “IMPORTANT HEALTH COVERAGE
TAX DOCUMENTS”; (2) explains how non-full-time employees
and non-employees who are enrolled in the plan may request a
copy of Form 1095-C; and (3) includes the employer’s email
address, mailing address, and telephone number.
•
The employer must post the notice on its website by March 1,
2024, and retain the notice in the same location on its website
through October 15, 2024.
•
The employer must furnish the statement to a requesting
individual within 30 days of the date the request is received. To
-6-
Instructions for Forms 1094-C and 1095-C (2023)

Page 7 of 18 Fileid: … 094c&1095c/2023/a/xml/cycle04/source 9:16 - 26-Sep-2023
The type and rule above prints on all proofs including departmental reproduction proofs. MUST be removed before printing.
satisfy this requirement, the employer may furnish the statement
electronically if the recipient affirmatively consents.
Specific Instructions for Form 1094-C
Part I—Applicable Large Employer Member
(ALE Member)
Line 1. Enter employer's name. The employer is the ALE
Member.
Line 2. Enter the ALE Member’s EIN. Do not enter an SSN.
Enter the 9-digit EIN, including the dash.
If you are filing Form 1094-C, a valid EIN is required at
the time the form is filed. If a valid EIN is not provided,
Form 1094-C will not be processed. If you do not have
an EIN, you may apply for one online. Go to
IRS.gov/EIN. You
may also apply by faxing or mailing Form SS-4, Application for
Employer Identification Number, to the IRS. See the Instructions
for Form SS-4 and Pub. 1635, Employer Identification Number.
Lines 3–6. Enter the ALE Member’s complete address
(including room or suite no., if applicable). This address should
match the ALE Member’s address used on Form 1095-C.
Lines 7 and 8. Enter the name and telephone number of the
person to contact who is responsible for answering any
questions from the IRS regarding the filing of, or information
reported on, Form 1094-C or 1095-C. This may be different than
the contact information on line 10 of Form 1095-C.
Note. If you are a Designated Governmental Entity (DGE) filing
on behalf of an ALE Member, complete lines 9–16. If you are not
a DGE filing on behalf of an ALE Member, do not complete lines
9–16. Instead, skip to line 18. See
Designated Governmental
Entity (DGE) in the Definitions section of these instructions.
Line 9. If a DGE is filing on behalf of the ALE Member, enter the
name of the DGE.
Line 10. Enter the DGE’s EIN (including the dash). Do not enter
an SSN.
If you are a DGE that is filing Form 1094-C, a valid EIN is
required at the time the return is filed. If a valid EIN is not
provided, the return will not be processed. If the DGE
does not have an EIN when filing Form 1094-C, it can get an EIN
by applying online at
IRS.gov/EIN or by faxing or mailing a
completed Form SS-4. See the Instructions for Form SS-4 and
Pub. 1635.
Lines 11–14. Enter the DGE’s complete address (including
room or suite no.).
Lines 15 and 16. Enter the name and telephone number of the
person to contact who is responsible for answering any
questions from the IRS regarding the filing of, or information
reported on, Form 1094-C.
Line 17. Reserved for future use.
Line 18. Enter the total number of Forms 1095-C submitted with
this Form 1094-C transmittal.
Line 19. If this Form 1094-C transmittal is the Authoritative
Transmittal that reports aggregate employer-level data for the
ALE Member, check the box on line 19 and complete Parts II, III,
and IV, to the extent applicable. Otherwise, complete the
signature portion of Form 1094-C and leave the remainder of
Parts II, III, and IV blank.
There must be only one Authoritative Transmittal filed for each
ALE Member. If this is the only Form 1094-C being filed for the
ALE Member, this Form 1094-C must report aggregate
CAUTION
!
CAUTION
!
employer-level data for the ALE Member and be identified on
line 19 as the Authoritative Transmittal. If multiple Forms 1094-C
are being filed for an ALE Member so that Forms 1095-C for all
full-time employees of the ALE Member are not attached to a
single Form 1094-C transmittal (because Forms 1095-C for
some full-time employees of the ALE Member are being
transmitted separately), one (and only one) of the Forms 1094-C
must report aggregate employer-level data for the ALE Member
and be identified on line 19 as the Authoritative Transmittal. For
more information, see
Authoritative Transmittal for ALE Members
Filing Multiple Forms 1094-C, earlier.
Part II—ALE Member Information
Reminder. Lines 20–22 should be completed only on the
Authoritative Transmittal for the ALE Member. For more
information, see Authoritative Transmittal for ALE Members Filing
Multiple Forms 1094-C, earlier.
Line 20. Enter the total number of Forms 1095-C that will be
filed by, and/or on behalf of, the ALE Member. This includes all
Forms 1095-C that are filed with this transmittal, including those
filed for individuals who enrolled in the employer-sponsored,
self-insured plan, if any, and for any Forms 1095-C filed with a
separate transmittal filed by, or on behalf of, the ALE Member.
Line 21. If during any month of the calendar year the ALE
Member was a member of an Aggregated ALE Group, check
“Yes.” If you check “Yes,” also complete the “Aggregated Group
Indicator” in Part III, column (d), and then complete Part IV to list
the other members of the Aggregated ALE Group. If, for all 12
months of the calendar year, the employer was not a member of
an Aggregated ALE Group, check “No,” and do not complete
Part III, column (d), or Part IV.
Line 22. If the ALE Member meets the eligibility requirements
and is using one of the Offer Methods, it must check the
applicable box. See the descriptions of Qualifying Offer Method
and 98% Offer Method, later.
A. Qualifying Offer Method. Check this box if the ALE
Member is eligible to use, and is using, the Qualifying Offer
Method to report the information on Form 1095-C for one or
more full-time employees. Under the Qualifying Offer Method,
there is an alternative method of completing Form 1095-C and
an alternative method for furnishing Form 1095-C to certain
employees. If the ALE Member is using either of these
alternative rules, check this box. To be eligible to use the
Qualifying Offer Method, the ALE Member must certify that it
made a Qualifying Offer to one or more of its full-time employees
for all months during the year in which the employee was a
full-time employee for whom an employer shared responsibility
payment could apply. Additional requirements described below
must be met to be eligible to use the alternative method for
furnishing Form 1095-C to employees under the Qualifying Offer
Method.
Alternative method of completing Form 1095-C under
the Qualifying Offer Method. If the ALE Member reports using
this method, it must not complete Form 1095-C, Part II, line 15,
for any month for which a Qualifying Offer is made. Instead, it
must enter the Qualifying Offer code 1A on Form 1095-C,
line 14, for any month for which the employee received a
Qualifying Offer (or in the “ All 12 Months” box if the employee
received a Qualifying Offer for all 12 months), and must leave
line 15 blank for any month for which code 1A is entered on
line 14. The ALE Member may, but is not required to, enter an
applicable code on line 16 for any month for which code 1A is
entered on line 14; a Qualifying Offer is, by definition, treated as
an offer that falls within an affordability safe harbor even if no
code is entered on line 16.
An ALE Member is not required to use the Qualifying Offer
Method even if it is eligible, and instead may enter on line 14 the
Instructions for Forms 1094-C and 1095-C (2023)
-7-

Page 8 of 18 Fileid: … 094c&1095c/2023/a/xml/cycle04/source 9:16 - 26-Sep-2023
The type and rule above prints on all proofs including departmental reproduction proofs. MUST be removed before printing.
applicable offer code and then enter on line 15 the Employee
Required Contribution.
If the ALE Member is eligible to use the Qualifying Offer
Method, it may report on Form 1095-C by entering the
Qualifying Offer code 1A on Form 1095-C, line 14, for
any month for which it made a Qualifying Offer to an employee,
even if the employee did not receive a Qualifying Offer for all 12
calendar months. However, if an employee receives a Qualifying
Offer for less than all 12 months, the ALE Member must furnish a
copy of Form 1095-C to the employee (rather than using the
alternative method of furnishing Form 1095-C described later).
Example. Employee’s employment with Employer begins on
January 1. Employee is in a health coverage waiting period (and
an employer shared responsibility payment could not apply with
respect to Employee, because Employee is in a Limited
Non-Assessment Period) until April 1 and is a full-time employee
for the remainder of the calendar year. Employer makes a
Qualifying Offer to Employee for coverage beginning on April 1
and for the remainder of the calendar year. Employer is eligible
to use the Qualifying Offer method because it has made a
Qualifying Offer to at least one full-time employee for all months
in which both (1) the employee was a full-time employee, and (2)
an employer shared responsibility payment could apply with
respect to the employee. Employer may use the alternative
method of completing Form 1095-C under the Qualifying Offer
Method for this Employee. However, Employer may not use the
alternative method of furnishing Form 1095-C to Employee under
the Qualifying Offer Method because Employee did not receive a
Qualifying Offer for all 12 months of the calendar year.
Alternative method of furnishing Form 1095-C to
employees under the Qualifying Offer Method. An ALE
Member that is eligible to use the Qualifying Offer Method may
use the alternative method of furnishing Form 1095-C only for a
full-time employee who (1) received a Qualifying Offer for all 12
months of the calendar year, and (2) did not enroll in
employer-sponsored, self-insured coverage. For such an
employee, an ALE Member meets its obligation to furnish a Form
1095-C to the employee if it furnishes the employee a statement
containing the following information.
•
Employer/ALE Member name, address, and EIN.
•
Contact name and telephone number at which the employee
may receive information about the offer of coverage and the
information on the Form 1095-C filed with the IRS for that
employee.
•
Notification that, for all 12 months of the calendar year, the
employee and his or her spouse and dependents, if any,
received a Qualifying Offer and therefore the employee is not
eligible for a premium tax credit.
•
Information directing the employee to see Pub. 974, Premium
Tax Credit (PTC), for more information on eligibility for the
premium tax credit.
An ALE Member is not required to use the alternative method
of furnishing for an employee even if the alternative method
would be allowed. Instead, the ALE Member may furnish a copy
of Form 1095-C as filed with the IRS (with or without the
statement described earlier).
As stated earlier, an ALE Member may not use the alternative
furnishing method for a full-time employee who enrolled in
self-insured coverage. Rather, the ALE Member must furnish
Form 1095-C, including the information reporting enrollment in
the coverage on Form 1095-C, Part III.
B. Reserved for future use.
C. Reserved for future use.
D. 98% Offer Method. Check this box if the employer is
eligible for, and is using, the 98% Offer Method. To be eligible to
use the 98% Offer Method, an employer must certify that, taking
into account all months during which the individuals were
employees of the ALE Member and were not in a Limited
TIP
Non-Assessment Period, the ALE Member offered affordable
health coverage providing minimum value to at least 98% of its
employees for whom it is filing a Form 1095-C employee
statement, and offered minimum essential coverage to those
employees’ dependents. The ALE Member is not required to
identify which of the employees for whom it is filing were full-time
employees, but the ALE Member is still required, under the
general reporting rules, to file Forms 1095-C on behalf of all its
full-time employees who were full-time employees for one or
more months of the calendar year. To ensure compliance with
the general reporting rules, an ALE Member should confirm for
any employee for whom it fails to file a Form 1095-C that the
employee was not a full-time employee for any month of the
calendar year. For this purpose, the health coverage is affordable
if the ALE Member meets one of the section 4980H affordability
safe harbors.
Example. Employer has 325 employees. Of those 325
employees, Employer identifies 25 employees as not possibly
being full-time employees because they are scheduled to work
10 hours per week and are not eligible for additional hours. Of
the remaining 300 employees, 295 are offered affordable
minimum value coverage for all periods during which they are
employed other than any applicable waiting period (which
qualifies as a Limited Non-Assessment Period). Employer files a
Form 1095-C for each of the 300 employees (excluding the 25
employees that it identified as not possibly being full-time
employees). Employer may use the 98% Offer Method because
it makes an affordable offer of coverage that provides minimum
value to at least 98% of the employees for whom Employer files
a Form 1095-C. Using this method, Employer does not identify
whether each of the 300 employees is a full-time employee.
However, Employer must still file a Form 1095-C for all of its
full-time employees. Employer chooses to file a Form 1095-C on
behalf of all 300 employees, including the five employees to
whom it did not offer coverage, because if one or more of those
employees was, in fact, a full-time employee for one or more
months of the calendar year, Employer would be required to
have filed a Form 1095-C on behalf of those employees.
Note. If an ALE Member uses the 98% offer method, it is not
required to complete the “Section 4980H Full-Time Employee
Count for ALE Member” in Part III, column (b).
Part III—ALE Member Information—Monthly
(Lines 23–35)
Column (a)—Minimum Essential Coverage Offer Indicator.
•
If the ALE Member offered minimum essential coverage,
including an individual coverage HRA, to at least 95% of its
full-time employees and their dependents for the entire calendar
year, enter “X” in the “Yes” checkbox on line 23 for “All 12
Months” or for each of the 12 calendar months.
•
If the ALE Member offered minimum essential coverage,
including an individual coverage HRA, to at least 95% of its
full-time employees and their dependents only for certain
calendar months, enter “X” in the “Yes” checkbox for each
applicable month.
•
For the months, if any, for which the ALE Member did not offer
minimum essential coverage, including an individual coverage
HRA, to at least 95% of its full-time employees and their
dependents, enter “X” in the “No” checkbox for each applicable
month.
•
If the ALE Member did not offer minimum essential coverage,
including an individual coverage HRA, to at least 95% of its
full-time employees and their dependents for any of the 12
months, enter “X” in the “No” checkbox for “All 12 Months” or for
each of the 12 calendar months.
Note. For purposes of column (a), an employee in a Limited
Non-Assessment Period is not counted in determining whether
-8-
Instructions for Forms 1094-C and 1095-C (2023)
Page 9 of 18 Fileid: … 094c&1095c/2023/a/xml/cycle04/source 9:16 - 26-Sep-2023
The type and rule above prints on all proofs including departmental reproduction proofs. MUST be removed before printing.
minimum essential coverage was offered to at least 95% of an
ALE Member’s full-time employees and their dependents. For a
description of the differences between the definition of the term
“Limited Non-Assessment Period” used with respect to section
4980H(a) and the definition used with respect to section
4980H(b), relating to whether the ALE Member offers minimum
value coverage at the end of the Limited Non-Assessment
Period, see the
Definitions section.
An employee who is treated as having been offered
health coverage, including an individual coverage HRA,
for purposes of section 4980H (even though not actually
offered) is treated as offered minimum essential coverage for this
purpose. For example, for the months for which the ALE Member
is eligible for multiemployer arrangement interim guidance (if the
ALE Member is contributing on behalf of an employee whether
or not the employee is eligible for coverage under the
multiemployer plan) with respect to an employee, that employee
should be treated as having been offered minimum essential
coverage for purposes of column (a). For different rules for
purposes of reporting offers of coverage on Form 1095-C, see
the specific instructions for Form 1095-C, Part II,
line 14.
For purposes of column (a), if the ALE Member offered
minimum essential coverage to all but five of its full-time
employees and their dependents, and five is greater
than 5% of the number of full-time employees of the ALE
Member, the ALE Member may report in column (a) as if it
offered health coverage to at least 95% of its full-time employees
and their dependents (even if it offered health coverage to less
than 95% of its full-time employees and their dependents, for
example, to 75 of its 80 full-time employees and their
dependents).
See Definitions, later, for more information on an offer of
health coverage.
Column (b)—Section 4980H Full-Time Employee Count for
ALE Member. Enter the number of full-time employees for each
month, but do not count any employee in a Limited
Non-Assessment Period. If the number of full-time employees
(excluding employees in a Limited Non-Assessment Period) for a
month is zero, enter -0-. An employee should be counted as a
full-time employee for a month if the employee satisfied the
definition of “full-time employee” under the monthly
measurement method or the look-back measurement method
(as applicable) on any day of the month. See
Full-time employee
and Limited Non-Assessment Period in the Definitions section.
Be sure to use the section 4980H definition and not any other
definition of the term “full-time employee” that you may use for
other purposes.
Example. Employer uses the look-back measurement
method to determine the full-time status of its employees.
Employee, who is not in a Limited Non-Assessment Period,
averaged over 130 hours of service per month during the
measurement period that corresponds with the stability period
starting January 1, 2023, and ending December 31, 2023.
Employee terminates employment with Employer on February
15, 2023. Employer must include Employee in the number of
full-time employees reported in column (b) for January and
February. See the description of code 2B in the instructions for
line 16 of Form 1095-C, later, for rules for reporting an offer of
coverage in an employee’s final month of employment.
Note. If the ALE Member certified that it was eligible for the 98%
Offer Method by selecting box D, on line 22, it is not required to
complete column (b).
Column (c)—Total Employee Count for ALE Member. Enter
the total number of all of the ALE Member’s employees,
including full-time employees and non-full-time employees, and
TIP
TIP
employees in a Limited Non-Assessment Period, for each
calendar month. An ALE Member must choose to use one of the
following days of the month to determine the number of
employees per month and must use that day for all months of the
year: (1) the first day of each month, (2) the last day of each
month, (3) the 12th day of each month, (4) the first day of the first
payroll period that starts during each month, or (5) the last day of
the first payroll period that starts during each month (provided
that for each month that last day falls within the calendar month
in which the payroll period starts). If the total number of
employees was the same for every month of the entire calendar
year, enter that number in line 23, column (c), “All 12 Months,” or
in the boxes for each month of the calendar year. If the number
of employees for any month is zero, enter -0-.
Column (d)—Aggregated Group Indicator. An ALE Member
must complete this column if it checked “Yes” on line 21,
indicating that, during any month of the calendar year, it was a
member of an Aggregated ALE Group. If the ALE Member was a
member of an Aggregated ALE Group during each month of the
calendar year, enter “X” in the “All 12 Months” box or in the boxes
for each of the 12 calendar months. If the ALE Member was not
a member of an Aggregated ALE Group for all 12 months but
was a member of an Aggregated ALE Group for one or more
month(s), enter “X” in each month for which it was a member of
an Aggregated ALE Group. If an ALE Member enters “X” in one
or more months in this column, it must also complete Part IV.
Part IV—Other ALE Members of
Aggregated ALE Group (Lines 36–65)
An ALE Member must complete this section if it checks “Yes” on
line 21. If the ALE Member was a member of an Aggregated ALE
Group (with other ALE Members) for any month of the calendar
year, enter the name(s) and EIN(s) of up to 30 of the other
Aggregated ALE Group members (not including the reporting
ALE Member). If there are more than 30 members of the
Aggregated ALE Group (not including the reporting ALE
Member), enter the 30 with the highest monthly average number
of full-time employees (using the number reported in Part III,
column (b), if a number was required to be reported) for the year
or for the number of months during which the ALE Member was
a member of the Aggregated ALE Group. If any member of the
Aggregated ALE Group uses the 98% Offer Method and thus is
not required to identify which employees are full-time employees,
all ALE Members of the Aggregated ALE Group should use the
monthly average number of total employees rather than the
monthly average number of full-time employees for this purpose.
Regardless of the number of members in the Aggregated ALE
Group, list only the 30 members in descending order, listing first
the member with the highest average monthly number of full-time
employees (or highest average number of total employees, if any
member of the Aggregated ALE Group uses the 98% Offer
Method), but do not include the reporting ALE Member. The
reporting ALE Member must also complete Part III, column (d),
to indicate which months it was part of an Aggregated ALE
Group.
If you are filing Form 1094-C, a valid EIN is required at
the time it is filed. If a valid EIN is not provided, Form
1094-C will not be processed. If you do not have an EIN,
you may apply for one online. Go to IRS.gov/EIN. You may also
apply by faxing or mailing Form SS-4 to the IRS. See the
Instructions for Form SS-4 and Pub. 1635.
CAUTION
!
Instructions for Forms 1094-C and 1095-C (2023)
-9-

Page 10 of 18 Fileid: … 094c&1095c/2023/a/xml/cycle04/source 9:16 - 26-Sep-2023
The type and rule above prints on all proofs including departmental reproduction proofs. MUST be removed before printing.
Specific Instructions for Form 1095-C
Part I—Employee
Line 1. Enter the name of the employee (first name, middle
initial, last name).
Line 2. Enter the 9-digit SSN of the employee (including the
dashes).
Lines 3–6. Enter the employee’s complete address, including
apartment no., if applicable. A country code is not required for
U.S. addresses.
Part I—Applicable Large Employer Member
(Employer)
Line 7. Enter the name of the ALE Member.
Line 8. Enter the ALE Member’s EIN. Do not enter an SSN.
Enter the 9-digit EIN, including the dash. The ALE Member’s
name and EIN should match the name and EIN of the ALE
Member reported on lines 1 and 2 of Form 1094-C.
If you are filing Form 1095-C, a valid EIN is required at
the time it is filed. If a valid EIN is not provided, Form
1095-C will not be processed. If you do not have an EIN,
you may apply for one online. Go to
IRS.gov/EIN. You may also
apply by faxing or mailing Form SS-4 to the IRS. See the
Instructions for Form SS-4 and Pub. 1635.
Lines 9 and 11–13. Enter the ALE Member’s complete address
(including room or suite no., if applicable). This address should
match the address reported on lines 3–6 of the Form 1094-C.
Line 10. Enter the telephone number of the person to contact
whom the recipient may call about the information reported on
the form. This may be different than the contact information
entered on line 8 of Form 1094-C.
Part II—Employee Offer of Coverage
Age. If the employee was offered an individual coverage HRA,
enter the employee’s age on January 1, 2023. Note that for
non-calendar year plans or for employees who become eligible
during the plan year, this age may not be the Applicable age
used to determine Employee Required Contribution.
Plan Start Month. This box is required for the 2023 Form
1095-C and the ALE Member may not leave it blank. To
complete the box, enter the 2-digit number (01 through 12)
indicating the calendar month during which the plan year begins
of the health plan in which the employee is offered coverage (or
would be offered coverage if the employee were eligible to
participate in the plan). If more than one plan year could apply
(for instance, if the ALE Member changes the plan year during
the year), enter the earliest applicable month. If there is no health
plan under which coverage is offered to the employee, enter “00.”
Line 14. For each calendar month, enter the applicable code
from Code Series 1. If the same code applies for all 12 calendar
months, you may enter the applicable code in the “All 12 Months”
box and not complete the individual calendar month boxes, or
you may enter the code in each of the boxes for the 12 calendar
months. If an employee was not offered coverage for a month,
enter code 1H. Do not leave line 14 blank for any month
(including months when the individual was not an employee of
the ALE Member). An ALE Member offers health coverage for a
month only if it offers health coverage that would provide
coverage for every day of that calendar month. Thus, if coverage
terminates before the last day of the month (because, for
instance, the employee terminates employment with the ALE
Member, or otherwise loses eligibility for coverage under the
CAUTION
!
plan), the employee does not actually have an offer of coverage
for that month (and code 1H should therefore be entered on
line 14). See line 16, code 2B, later, for how the ALE Member
may complete line 16 in the event that coverage terminates
before the last day of the month.
A code must be entered for each calendar month, January
through December, even if the employee was not a full-time
employee for one or more of the calendar months. Enter the
code identifying the type of health coverage actually offered by
the ALE Member (or on behalf of the ALE Member) to the
employee, if any. If the employee was not actually offered
coverage, enter code 1H (no offer of coverage) on line 14.
For reporting offers of coverage for 2023, an ALE Member
relying on the multiemployer arrangement interim guidance
should enter code 1H on line 14 for any month for which the ALE
Member enters code 2E on line 16 (indicating that the ALE
Member was required to contribute to a multiemployer plan on
behalf of the employee for that month and therefore is eligible for
multiemployer interim rule relief). For a description of the
multiemployer arrangement interim guidance, see
Offer of health
coverage in the Definitions section. For reporting for 2023, code
1H may be entered without regard to whether the employee was
eligible to enroll, or enrolled in, coverage under the
multiemployer plan. For reporting for 2024 and future years, ALE
Members relying on the multiemployer arrangement interim
guidance may be required to report offers of coverage made
through a multiemployer plan in a different manner.
Indicator Codes for Employee Offer of Coverage
(Form 1095-C, Line 14)
Code Series 1—Offer of Coverage. The Code Series 1
indicator codes specify the type of coverage, if any, offered to an
employee, the employee’s spouse, and the employee’s
dependents. The term
Dependent has the specific meaning set
forth in the Definitions section of these instructions. In addition,
for this purpose, an offer of coverage is treated as made to an
employee’s dependents only if the offer of coverage is made to
an unlimited number of dependents regardless of the actual
number of dependents, if any, an employee has during any
particular calendar month.
If the type of coverage, if any, offered to an employee was the
same for all 12 months in the calendar year, enter the Code
Series 1 indicator code corresponding to the type of coverage
offered either in the “All 12 Months” box or in each of the 12
boxes for the calendar months.
Conditional offer of spousal coverage. Codes 1J and 1K
address conditional offers of spousal coverage (also referred to
as “coverage offered conditionally”). A conditional offer is an
offer of coverage that is subject to one or more reasonable,
objective conditions (for example, an offer to cover an
employee’s spouse only if the spouse is not eligible for coverage
under Medicare or a group health plan sponsored by another
employer). Using codes 1J and 1K, an ALE Member may report
a conditional offer to a spouse as an offer of coverage,
regardless of whether the spouse meets the reasonable,
objective condition. A conditional offer may impact a spouse's
eligibility for the premium tax credit under section 36B only if all
conditions to the offer are satisfied (that is, the spouse was
actually offered the coverage and eligible for it) and the
Exchange makes a determination about the affordability of the
offer. To help employees (and spouses) who have received a
conditional offer determine their eligibility for the premium tax
credit, the ALE Member should be prepared to provide, upon
request, a list of any and all conditions applicable to the spousal
offer of coverage. As is noted in the definition of
Dependent in
the Definitions section, a spouse is not a dependent for
purposes of section 4980H.
-10-
Instructions for Forms 1094-C and 1095-C (2023)
Page 11 of 18 Fileid: … 094c&1095c/2023/a/xml/cycle04/source 9:16 - 26-Sep-2023
The type and rule above prints on all proofs including departmental reproduction proofs. MUST be removed before printing.
An ALE Member may not report a conditional offer of
coverage to an employee’s dependents as an offer to the
dependents, unless the ALE Member knows that the
dependents met the condition to be eligible for the ALE
Member’s coverage. Further, an offer of coverage is treated as
made to an employee’s dependents only if the offer of coverage
is made to an unlimited number of dependents regardless of the
actual number of dependents, if any, an employee has during
any particular calendar month.
COBRA continuation coverage. An offer of COBRA
continuation coverage is reported differently depending on
whether or not the offer is made due to an employee’s
termination of employment.
An offer of COBRA continuation coverage that is made to a
former employee (or to a former employee’s spouse or
dependents) due to termination of employment should not be
reported as an offer of coverage on line 14. In this situation, code
1H (No offer of coverage) must be entered on line 14 for any
month for which the offer of COBRA continuation coverage
applies, and code 2A (Employee not employed during the
month) must be entered on line 16 (see the instructions for
line 16), without regard to whether the employee or spouse or
dependents enrolled in the COBRA coverage. However, for the
month in which the employee terminates employment with the
ALE Member, see the instructions for line 16, code 2B.
An offer of COBRA continuation coverage that is made to an
employee who remains employed by the ALE Member (or to that
employee’s spouse and dependents) should be reported on
line 14 as an offer of coverage, but only for any individual who
receives an offer of COBRA continuation coverage (or an offer of
similar coverage that is made at the same time as the offer of
COBRA continuation coverage is made to enrolled individuals).
Generally, an offer of COBRA continuation coverage is required
to be made only to individuals who were enrolled in coverage
and would lose eligibility for coverage due to the COBRA
qualifying event, but an ALE Member may choose to extend a
similar offer of coverage to a spouse or dependent even if the
offer is not required by COBRA.
Example. During the applicable open enrollment period for
its health plan, Employer makes an offer of minimum essential
coverage providing minimum value to Employee and to
Employee’s spouse and dependents. Employee elects to enroll
in employee-only coverage starting January 1. On June 1,
Employee experiences a reduction in hours that results in loss of
eligibility for coverage under the plan. As of June 1, Employer
terminates Employee’s existing coverage and makes an offer of
COBRA continuation coverage to Employee, but does not make
an offer to Employee’s spouse and dependents. Employer
should enter code 1E (Minimum essential coverage providing
minimum value offered to employee and at least minimum
essential coverage offered to dependent(s) and spouse) on
line 14 for months January–May, and should enter code 1B
(Minimum essential coverage providing minimum value offered
to employee only) on line 14 for months June–December.
Note. Notwithstanding the preceding instructions for completing
line 14 of Form 1095-C, for purposes of section 4980H, an ALE
Member is treated as having made an offer to the employee’s
dependents for an entire plan year if the ALE Member provided
the employee an effective opportunity to enroll the employee’s
dependents at least once for the plan year, even if the employee
declined to enroll the dependents in the coverage and, as a
result, the dependents later did not receive an offer of COBRA
coverage.
Post-employment (non-COBRA) coverage. An offer of
post-employment coverage to a former employee (or to that
former employee’s spouse or dependent(s)) for coverage that
would be effective after the employee has terminated
employment (such as at retirement) should not be reported as an
offer of coverage on line 14. If the ALE Member is otherwise
required to file Form 1095-C for the former employee (because,
for example, the individual was a full-time employee for one or
more months in the calendar year in which the termination of
employment occurred), the ALE Member should enter code 1H
(no offer of coverage) on line 14 for any month to which an offer
of post-employment coverage applies, and should also enter
code 2A (not an employee) on line 16 (see the instructions for
line 16).
For additional information, including examples about
reporting offers of COBRA continuation coverage and
post-employment coverage, go to IRS.gov/Affordable-
Care-Act/Employers/Questions-and-Answers-about-Information-
Reporting-by-Employers-on-Form-1094-C-and-Form-1095-C.
•
1A. Qualifying Offer: Minimum essential coverage providing
minimum value offered to full-time employee with Employee
Required Contribution equal to or less than 9.5% (as adjusted) of
mainland single federal poverty line and at least minimum
essential coverage offered to spouse and dependent(s).
This code may be used to report for specific months for
which a Qualifying Offer was made, even if the employee
did not receive a Qualifying Offer for all 12 months of the
calendar year. However, an ALE Member may not use the
Alternative Furnishing Method for an employee who did not
receive a Qualifying Offer for all 12 calendar months.
•
1B. Minimum essential coverage providing minimum value
offered to employee only.
•
1C. Minimum essential coverage providing minimum value
offered to employee and at least minimum essential coverage
offered to dependent(s) (not spouse).
•
1D. Minimum essential coverage providing minimum value
offered to employee and at least minimum essential coverage
offered to spouse (not dependent(s)). Do not use code 1D if the
coverage for the spouse was offered conditionally. Instead, use
code 1J.
•
1E. Minimum essential coverage providing minimum value
offered to employee and at least minimum essential coverage
offered to dependent(s) and spouse. Do not use code 1E if the
coverage for the spouse was offered conditionally. Instead, use
code 1K.
•
1F. Minimum essential coverage NOT providing minimum
value offered to employee; employee and spouse or
dependent(s); or employee, spouse, and dependents.
•
1G. Offer of coverage for at least one month of the calendar
year to an individual who was not an employee for any month of
the calendar year or to an employee who was not a full-time
employee for any month of the calendar year (which may include
one or more months in which the individual was not an
employee) and who enrolled in self-insured coverage for one or
more months of the calendar year.
Note. Code 1G applies for the entire year or not at all.
Therefore, if code 1G applies, an ALE Member must enter code
1G on line 14 in the “All 12 Months” column or in each separate
monthly box (for all 12 months).
•
1H. No offer of coverage (employee not offered any health
coverage or employee offered coverage that is not minimum
essential coverage, which may include one or more months in
which the individual was not an employee).
•
1I. Reserved for future use.
•
1J. Minimum essential coverage providing minimum value
offered to employee and at least minimum essential coverage
conditionally offered to spouse; minimum essential coverage not
offered to dependent(s). (See Conditional offer of spousal
coverage, earlier, for an additional description of conditional
offers.)
•
1K. Minimum essential coverage providing minimum value
offered to employee; at least minimum essential coverage
TIP
TIP
Instructions for Forms 1094-C and 1095-C (2023)
-11-

Page 12 of 18 Fileid: … 094c&1095c/2023/a/xml/cycle04/source 9:16 - 26-Sep-2023
The type and rule above prints on all proofs including departmental reproduction proofs. MUST be removed before printing.
offered to dependents; and at least minimum essential coverage
conditionally offered to spouse. (See Conditional offer of spousal
coverage, earlier, for an additional description of conditional
offers.)
•
1L. Individual coverage HRA offered to employee only with
affordability determined by using employee’s primary residence
location ZIP code.
•
1M. Individual coverage HRA offered to employee and
dependent(s) (not spouse) with affordability determined by using
employee’s primary residence location ZIP code.
•
1N. Individual coverage HRA offered to employee, spouse,
and dependent(s) with affordability determined by using
employee’s primary residence location ZIP code.
•
1O. Individual coverage HRA offered to employees only using
the employee’s primary employment site ZIP code affordability
safe harbor.
•
1P. Individual coverage HRA offered to employee and
dependent(s) (not spouse) using the employee’s primary
employment site ZIP code affordability safe harbor.
•
1Q. Individual coverage HRA offered to employee, spouse,
and dependent(s) using employee’s primary employment site
ZIP code affordability safe harbor.
•
1R. Individual coverage HRA that is NOT affordable offered to
employee; employee and spouse, or dependent(s); or employee,
spouse, and dependents.
•
1S. Individual coverage HRA offered to an individual who was
not a full-time employee.
•
1T. Individual coverage HRA offered to employee and spouse
(not dependents) with affordability determined using employee's
primary residence location ZIP code.
•
1U. Individual coverage HRA offered to employee and spouse
(not dependents) using employee's primary employment site ZIP
code affordability safe harbor.
•
1V. Reserved for future use.
•
1W. Reserved for future use.
•
1X. Reserved for future use.
•
1Y. Reserved for future use.
•
1Z. Reserved for future use.
Line 15. Complete line 15 only if code 1B, 1C, 1D, 1E, 1J, 1K,
1L, 1M, 1N, 1O, 1P, 1Q, 1T, or 1U is entered on line 14 either in
the “All 12 Months” box or in any of the monthly boxes. Enter the
amount of the Employee Required Contribution, which is,
generally, the employee share of the monthly cost for the
lowest-cost, self-only, minimum essential coverage providing
minimum value that is offered to the employee. For additional
details on how to determine the Employee Required
Contribution, including how to determine the Employee Required
Contribution for the individual coverage HRA, see the
Definitions
section, later. Enter the amount, including any cents. If the
employee is offered coverage but the Employee Required
Contribution is zero, enter “0.00” (do not leave blank). If the
Employee Required Contribution was the same amount for all 12
calendar months, you may enter that monthly amount in the “All
12 Months” box and not complete the monthly boxes. If the
Employee Required Contribution was not the same for all 12
months (for instance, if an ALE Member has a noncalendar year
plan and the employee share of the premium changes with the
new plan year that starts in 2023), enter the amount in each
calendar month for which the employee was offered minimum
value coverage. See the definition of
Employee Required
Contribution in the Definitions section, for more information,
including on how to determine the monthly required contribution
from annual data.
For line 15, the amount entered might not be the amount
the employee is paying for the coverage, for example, if
the employee chose to enroll in more expensive
coverage, such as family coverage, or if the employee is eligible
for certain other healthcare arrangements.
TIP
Line 16.
For each calendar month, enter the applicable code, if
any, from Code Series 2. Enter only one code from Code Series
2 per calendar month. The instructions below address which
code to use for a month if more than one code from Code Series
2 could apply. If the same code applies for all 12 calendar
months, you may enter the code in the “All 12 Months” box and
not complete the monthly boxes. If none of the codes apply for a
calendar month, leave the line blank for that month.
Code Series 2—Section 4980H Safe Harbor Codes and
Other Relief for ALE Members. An ALE Member enters the
applicable Code Series 2 indicator code, if any, on line 16 to
report for one or more months of the calendar year that one of
the following situations applied to the employee.
•
The employee was not employed or was not a full-time
employee,
•
The employee enrolled in the minimum essential coverage
offered,
•
The employee was in a Limited Non-Assessment Period with
respect to section 4980H(b),
•
The ALE Member met one of the section 4980H affordability
safe harbors with respect to this employee, or
•
The ALE Member was eligible for multiemployer interim rule
relief for this employee.
If no indicator code applies, leave line 16 blank. In some
circumstances, more than one indicator code could apply to the
same employee in the same month. For example, an employee
could be enrolled in health coverage for a particular month
during which he or she is not a full-time employee. However, only
one code may be used for a particular calendar month. For any
month in which an employee enrolled in minimum essential
coverage, in general, indicator code 2C reporting enrollment is
used instead of any other indicator code that could also apply
(but see the exceptions to this rule below regarding the
multiemployer interim rule relief and enrollment in COBRA
continuation coverage or other post-employment coverage). For
an employee who did not enroll in health coverage, there are
some specific ordering rules for which code to use. See the
descriptions of the codes.
Note. There is no code to enter on line 16 to indicate that a
full-time employee offered coverage either did not enroll in the
coverage or waived the coverage.
•
2A. Employee not employed during the month. Enter code 2A
if the employee was not employed on any day of the calendar
month. Do not use code 2A for a month if the individual was an
employee of the ALE Member on any day of the calendar month.
Do not use code 2A for the month during which an employee
terminates employment with the ALE Member.
•
2B. Employee not a full-time employee. Enter code 2B if the
employee is not a full-time employee for the month and did not
enroll in minimum essential coverage, if offered for the month.
Enter code 2B also if the employee is a full-time employee for the
month and whose offer of coverage (or coverage if the employee
was enrolled) ended before the last day of the month solely
because the employee terminated employment during the month
(so that the offer of coverage or coverage would have continued
if the employee had not terminated employment during the
month).
•
2C. Employee enrolled in health coverage offered. Enter code
2C for any month in which the employee enrolled for each day of
the month in health coverage offered by the ALE Member,
regardless of whether any other code in Code Series 2 might
also apply (for example, the code for a section 4980H
affordability safe harbor) except as provided below. Do not enter
code 2C on line 16 for any month in which the multiemployer
interim rule relief applies (enter code 2E). Do not enter code 2C
on line 16 if code 1G is entered on line 14. Do not enter code 2C
on line 16 for any month in which a terminated employee is
enrolled in COBRA continuation coverage or other
-12-
Instructions for Forms 1094-C and 1095-C (2023)
Page 13 of 18 Fileid: … 094c&1095c/2023/a/xml/cycle04/source 9:16 - 26-Sep-2023
The type and rule above prints on all proofs including departmental reproduction proofs. MUST be removed before printing.
post-employment coverage (enter code 2A). Do not enter code
2C on line 16 for any month in which the employee enrolled in
coverage that was not minimum essential coverage.
•
2D. Employee in a section 4980H(b) Limited Non-Assessment
Period. Enter code 2D for any month during which an employee
is in a section 4980H(b) Limited Non-Assessment Period. If an
employee is in an initial measurement period, enter code 2D
(employee in a section 4980H(b) Limited Non-Assessment
Period) for the month, and not code 2B (employee not a full-time
employee). For an employee in a section 4980H(b) Limited
Non-Assessment Period for whom the ALE Member is also
eligible for the multiemployer interim rule relief for the month,
enter code 2E (multiemployer interim rule relief) and not code 2D
(employee in a section 4980H(b) Limited Non-Assessment
Period).
•
2E. Multiemployer interim rule relief. Enter code 2E for any
month for which the multiemployer arrangement interim
guidance applies for that employee, regardless of whether any
other code in Code Series 2 (including code 2C) might also
apply. This relief is described under
Offer of Health Coverage in
the
Definitions section of these instructions.
Note. Although ALE Members may use the section 4980H
affordability safe harbors to determine affordability for purposes
of the multiemployer arrangement interim guidance, an ALE
Member eligible for the relief provided in the multiemployer
arrangement interim guidance for a month for an employee
should enter code 2E (multiemployer interim rule relief), and not
code 2F, 2G, or 2H (codes for section 4980H affordability safe
harbors).
•
2F. Section 4980H affordability Form W-2 safe harbor. Enter
code 2F if the ALE Member used the section 4980H Form W-2
safe harbor to determine affordability for purposes of section
4980H(b) for this employee for the year. If an ALE Member uses
this safe harbor for an employee, it must be used for all months
of the calendar year for which the employee is offered health
coverage.
•
2G. Section 4980H affordability federal poverty line safe
harbor. Enter code 2G if the ALE Member used the section
4980H federal poverty line safe harbor to determine affordability
for purposes of section 4980H(b) for this employee for any
month(s).
•
2H. Section 4980H affordability rate of pay safe harbor. Enter
code 2H if the ALE Member used the section 4980H rate of pay
safe harbor to determine affordability for purposes of section
4980H(b) for this employee for any month(s).
Note. An affordability safe harbor code should not be entered
on line 16 for any month that the ALE Member did not offer
minimum essential coverage, including an individual coverage
HRA, to at least 95% of its full-time employees and their
dependents (that is, any month for which the ALE Member
checked the “No” box on Form 1094-C, Part III, column (a)). For
more information, see the instructions for
Form 1094-C, Part III,
column (a).
•
2I. Reserved for future use.
Note. References to 9.5% in the section 4980H affordability
safe harbors and Qualifying Offer Method are applied based on
the percentage as indexed for purposes of applying the
affordability thresholds under section 36B (the premium tax
credit). The percentage, as adjusted, is 9.61% for plan years
beginning in 2022, and 9.12% for plan years beginning in 2023.
Line 17. If the ALE Member used code 1L, 1M, 1N, 1O, 1P, 1Q,
1T, or 1U because it offered the employee an individual coverage
HRA, enter the appropriate ZIP code used for identifying the
lowest cost silver plan used to calculate the Employee Required
Contribution in line 15. This will be the ZIP code of the
employee’s residence (code 1L, 1M, 1N, or 1T) or the ZIP code
of the employee’s primary site of employment if the ALE Member
uses the work location safe harbor (code 1O, 1P, 1Q, or 1U).
Location safe harbor for individual coverage HRAs. For
purposes of section 4980H(b), an employer may use the cost of
self-only coverage for the lowest cost silver plan for the
employee for self-only coverage offered through the Exchange
where the employee’s primary site of employment is located for
determining whether an offer of an individual coverage HRA to a
full-time employee is affordable. The ZIP code for the employee’s
primary site of employment is used to identify the applicable
lowest cost silver plan to determine affordability.
Part III—Covered Individuals (Lines 18–30)
Note. If there are more than 13 covered individuals, additional
copies of page 3, Part III, may be used.
Complete Part III ONLY if the ALE Member offers
employer-sponsored, self-insured health coverage, including an
individual coverage HRA, in which the employee or other
individual enrolled. For this purpose, employer-sponsored,
self-insured health coverage does not include coverage under a
multiemployer plan. Do not complete Part III if the ALE Member
offers coverage only under an insured group health plan. If an
ALE Member offers both insured and self-insured coverage,
complete Part III only for employees who enroll in the
self-insured coverage.
An ALE Member with a self-insured major medical plan and a
health reimbursement arrangement (HRA) that has an individual
who enrolls in both types of minimum essential coverage is
required to report the individual’s coverage under only one of the
arrangements in Part III. An ALE Member with an insured major
medical plan and an HRA that has an individual who enrolls in
both types of minimum essential coverage is not required to
report in Part III the HRA coverage of an individual if the
individual is eligible for the HRA because the individual enrolled
in the insured major medical plan. An ALE Member with an HRA
must report coverage under the HRA in Part III for any individual
who is not enrolled in a major medical plan of the ALE Member
(for example, if the individual is enrolled in a group health plan of
another employer (such as spousal coverage) or if the ALE
Member provides an individual coverage HRA). For additional
information on the reporting of supplemental coverage, see
Proposed Regulations section 1.6055-1(d)(2) and (3).
If the ALE Member is completing Part III, enter “X” in the
checkbox in Part III. If the ALE Member is not completing Part III,
do not enter “X” in the checkbox in Part III.
This part must be completed by an ALE Member offering
self-insured health coverage for any individual who was an
employee for one or more calendar months of the year, whether
full-time or non-full-time, and who enrolled in the coverage. The
employee (if enrolled in self-insured coverage) should be listed
on line 18; any other family members who enrolled in coverage
offered to the employee should be listed on subsequent lines.
All employee family members that are covered
individuals through the employee’s enrollment (for
example, because the employee elected family
coverage) must be included on the same form as the employee
(or any other individual to whom the offer was made). For
example, if the employee is offered family coverage by his or her
employer under a self-insured health plan and enrolls in the
family coverage, the employee and the employee’s family
members that are covered under the plan must all be reported
on the same Form 1095-C.
If two or more employees employed by the same ALE
Member are spouses or an employee and his or her dependent,
and one employee enrolled in a coverage option under the plan
that also covered the other employee(s) (for example, one
TIP
Instructions for Forms 1094-C and 1095-C (2023)
-13-
Page 14 of 18 Fileid: … 094c&1095c/2023/a/xml/cycle04/source 9:16 - 26-Sep-2023
The type and rule above prints on all proofs including departmental reproduction proofs. MUST be removed before printing.
employee spouse enrolled in family coverage that provided
coverage to the other employee spouse and their employee
dependent child), the enrollment information should be reflected
only on Form 1095-C for the employee who enrolled in the
coverage. (However, it would report the other employee family
members as covered individuals.)
Coverage of non-employee. This part may be completed by
an ALE Member offering self-insured health coverage for any
other individual who enrolled in the coverage under the plan for 1
or more calendar months of the year but was not an employee
for any calendar month of the year, such as a non-employee
director, a retired employee who retired in a previous year, a
terminated employee receiving COBRA continuation coverage
(or any other form of post-employment coverage) who
terminated employment during a previous year, and a
non-employee COBRA beneficiary (but not including an
individual who obtained coverage through the employee’s
enrollment, such as a spouse or dependent obtaining coverage
when an employee elects COBRA continuation coverage that is
family coverage). If Form 1095-C is used with respect to an
individual who was not an employee for any month of the
calendar year, Part II must be completed by using code 1G in the
“All 12 Months” box or the separate monthly boxes for all 12
calendar months. The employer must report for these individuals
using Form 1095-B, if it chooses not to use Form 1095-C.
If a non-employee individual enrolls in the coverage
under a self-insured health plan, all family members that
are covered individuals because of the individual’s
enrollment must be included on the same Form 1095-B or Form
1095-C as the individual who is offered, and enrolls in, the
coverage.
Columns (a) through (e), as applicable, must be completed
for each individual enrolled in the coverage, including the
employee reported on line 1. Enter the 9-digit SSN or other TIN
for each covered individual in column (b). Enter a date of birth in
column (c) only if an SSN or other TIN is not entered in column
(b). Column (d) will be checked if the individual was covered for
at least 1 day in every month of the year. For individuals who
were covered for some but not all months, information will be
entered in column (e) indicating the months for which these
individuals were covered.
Governmental Unit employers offering self-insured
health coverage that have delegated another
Governmental Unit (DGE) for purposes of reporting and
furnishing enrollment information (meaning the information that
otherwise would be reported on Form 1095-C, Part III), but have
not designated a DGE for purposes of reporting and furnishing
offer of coverage information (meaning the information that is
reported on Form 1095-C, Part II), should file and furnish Forms
1095-C with a completed Part I and Part II, but not a completed
Part III, and should not check the box indicating that the
Governmental Unit offers self-insured health coverage. In this
case, the DGE should file Forms 1094-B and 1095-B to report
enrollment information for employees on behalf of the
Governmental Unit. See FAQs on IRS.gov.
A DGE that has been delegated by a Governmental Unit for
purposes of reporting and furnishing both offer of coverage and
enrollment information (meaning the information that would be
reported on Parts II and III of Form 1095-C) should file Forms
1094-C and 1095-C to report the information for employees on
behalf of the Governmental Unit.
Column (a). Enter the name of each covered individual (first
name, middle initial, last name), including the employee, if the
employee is enrolled in self-insured coverage.
Column (b). Enter the 9-digit SSN for each covered individual,
including the dashes. For covered individuals who are not the
TIP
TIP
employee listed in Part I, a taxpayer identification number (TIN),
rather than an SSN, may be entered if the covered individual
does not have an SSN, or the field may be left blank if the
covered individual does not have a TIN.
Column (c). Enter a date of birth (YYYY-MM-DD) for the
covered individual only if column (b) is blank.
Column (d). Check this box if the individual was covered for at
least one day per month for all 12 months of the calendar year.
Column (e). If the individual was not covered for all 12 months
of the calendar year, check the applicable box(es) for the
month(s) in which the individual was covered for at least 1 day in
the month.
Definitions
This section contains the definitions of key terms used in Forms
1094-C and 1095-C and these instructions. For definitions of
terms not included in this section, see the final regulations under
section 4980H, T.D. 9655, 2014-9 I.R.B. 541, at
IRS.gov/irb/
2014-9_IRB/ar05.html and section 6056, T.D. 9661, 2014-13
I.R.B. 855, at IRS.gov/irb/2014-13_IRB/ar09.html.
Affordability. Generally, the lowest cost silver plan for the
employee based on the employee’s residence is used to
determine affordability. The ZIP code for the employee’s
residence is used to identify the applicable lowest cost silver
plan to determine affordability.
Aggregated ALE Group. An Aggregated ALE Group refers to a
group of ALE Members treated as a single employer under
section 414(b), 414(c), 414(m), or 414(o). An ALE Member is a
member of an Aggregated ALE Group for a month if it is treated
as a single employer with the other members of the group on any
day of the calendar month. If an ALE is made up of only one
person or entity, that one ALE Member is not a part of an
Aggregated ALE Group. Government entities and churches or
conventions or associations of churches may apply a
reasonable, good faith interpretation of the aggregation rules
under section 414 in determining their status as an ALE or
member of an Aggregated ALE Group. For more information on
how the aggregation rules apply to government entity employers,
see Notice 2015-87, Q&A 18, at
IRS.gov/irb/2015-52_IRB/
ar11.html.
Applicable Large Employer (ALE). An ALE is, for a particular
calendar year, any single employer, or group of employers
treated as an Aggregated ALE Group, that employed an average
of at least 50 full-time employees (including full-time equivalent
employees) on business days during the preceding calendar
year. For purposes of determining an employer’s average
number of employees, disregard an employee for any month in
which the employee has coverage under a plan described in
section 4980H(c)(2)(F) (generally, TRICARE or Veterans
Administration coverage). A new employer (that is, an employer
that was not in existence on any business day in the prior
calendar year) is an ALE for the current calendar year if it
reasonably expects to employ, and actually does employ, an
average of at least 50 full-time employees (including full-time
equivalent employees) on business days during the current
calendar year. For information on a special rule for certain
employers with seasonal workers, see the final regulations under
section 4980H and FAQs on IRS.gov.
Applicable Large Employer Member (ALE Member). An
ALE Member is a single person or entity that is an ALE, or if
applicable, each person or entity that is a member of an
Aggregated ALE Group. A person or entity that does not have
employees or only has employees with no hours of service (for
example, only employees whose entire service consists of work
-14-
Instructions for Forms 1094-C and 1095-C (2023)
Page 15 of 18 Fileid: … 094c&1095c/2023/a/xml/cycle04/source 9:16 - 26-Sep-2023
The type and rule above prints on all proofs including departmental reproduction proofs. MUST be removed before printing.
outside of the United States that does not count as hours of
service under section 4980H) is not an ALE Member.
Bona fide volunteer. A bona fide volunteer is an employee of a
government entity or tax-exempt organization whose only
compensation from that entity or organization is (1)
reimbursement for (or reasonable allowance for) reasonable
expenses incurred in the performance of services by volunteers,
or (2) reasonable benefits (including length of service awards),
and nominal fees, customarily paid by similar entities in
connection with the performance of services by volunteers.
COBRA continuation coverage. COBRA continuation
coverage is health coverage that is required to be offered under
the Consolidated Omnibus Budget Reconciliation Act of 1986
(COBRA) in certain circumstances in which an employee or
other individual covered under a health plan loses eligibility for
coverage under that health plan (for example, because the
employee terminates employment or has a reduction in hours).
For purposes of these instructions, COBRA continuation
coverage also includes coverage required under any other
federal or state law that provides continuation coverage
comparable to that provided under COBRA. For additional
details, see section 4980B and Regulations sections 54.4980B-1
through 54.4980B-10.
Dependent. A dependent is an employee’s child, including a
child who has been legally adopted or legally placed for adoption
with the employee, who has not reached age 26. A child reaches
age 26 on the 26th anniversary of the date the child was born
and is treated as a dependent for the entire calendar month
during which he or she reaches age 26. For this purpose, a
dependent does not include stepchildren, foster children, or a
child that does not reside in the United States (or a country
contiguous to the United States) and who is not a United States
citizen or national. For this purpose, a dependent does not
include a spouse.
Designated Governmental Entity (DGE). A DGE is a person
or persons that are part of or related to the Governmental Unit
that is the ALE Member and that is appropriately designated for
purposes of these reporting requirements. For a Governmental
Unit that has delegated some or all of its reporting
responsibilities to a DGE for some or all of its employees, one
Authoritative Transmittal must still be filed for that Governmental
Unit reporting aggregate employer-level data for all employees of
the Governmental Unit (including those for whom the
Governmental Unit has delegated its reporting responsibilities).
For more information, see
Authoritative Transmittal for Employers
Filing Multiple Forms 1094-C, earlier.
Eligible employer-sponsored plan. An eligible
employer-sponsored plan refers to group health coverage for
employees under (1) a governmental plan, such as the Federal
Employees Health Benefits Program (FEHB); (2) an insured plan
or coverage offered in the small or large group market within a
state; (3) a grandfathered health plan offered in a group market;
or (4) a self-insured group health plan for employees, including
an individual coverage HRA.
Employee. An employee is an individual who is an employee
under the common-law standard for determining employer–
employee relationships. An employee does not include a sole
proprietor, a partner in a partnership, an S corporation
shareholder who owns at least 2% of the S corporation, a leased
employee within the meaning of section 414(n), or a worker that
is a qualified real estate agent or direct seller.
If an employee is an employee of more than one ALE Member
of the same Aggregated ALE Group during a calendar month,
the employee is treated as an employee of the ALE Member for
whom the employee has the greatest number of hours of service
for that calendar month; if the employee has an equal number of
hours of service for two or more ALE Members of the same
Aggregated ALE Group for the calendar month, those ALE
Members must treat one of the ALE Members as the employer of
that employee for that calendar month. See One Form 1095-C
for Each Employee of Each Employer for a discussion of
reporting in these circumstances. See Pub.15-A, Employer’s
Supplemental Tax Guide, for more information on determining
who is an employee.
Note. In certain circumstances, an employee may have a
break in service (including a break in service due to a
termination of employment) during which the individual does not
earn hours of service but, upon beginning to earn hours of
service again, the ALE Member must treat the individual as a
continuing employee rather than a new hire for purposes of
certain rules under the regulations under section 4980H. See
Regulations sections 54.4980H-3(c)(4) and 54.4980H-3(d)(6).
These rules do not impact whether the individual was an
employee during the break in service, so the individual should
only be treated as an employee during the break in service for
purposes of reporting if the individual remained an employee
during that period (and had not terminated employment with the
ALE Member). For example, an employee on unpaid leave
during the break in service would be treated as an employee for
reporting purposes during the break in service, while a former
employee whose employment had been terminated during the
break in service would not be treated as an employee for
reporting purposes.
Employee Required Contribution. The Employee Required
Contribution is the employee’s share of the monthly cost for the
lowest-cost, self-only minimum essential coverage providing
minimum value that is offered to the employee by the ALE
Member. The employee share is the portion of the monthly cost
that would be paid by the employee for self-only coverage,
whether paid through salary reduction or otherwise.
For purposes of determining the amount of the employee’s
share of the monthly cost, an ALE Member may divide the total
cost to the employee for the plan year by the number of months
in the plan year. This monthly amount of the employee’s share of
the cost would then be reported for any months of that plan year
that fall within the 2023 calendar year. For example, if the plan
year begins January 1, the ALE Member may determine the
amount to report for each month by taking the total annual
employee cost for all 12 months and dividing by 12. If the plan
year begins April 1, the ALE Member may determine the amount
to report for January through March 2023, by taking the total
annual employee cost for the plan year ending March 31, 2023,
and dividing by 12 (and reporting that amount for January,
February, and March 2023). Then, the ALE Member may
determine the monthly amount for April through December 2023
by taking the total annual employee cost for the plan year ending
March 31, 2023, and dividing by 12 (and reporting that amount
for April through December 2023).
The Employee Required Contribution may not be the amount
the employee paid for coverage. For additional rules on
determining the amount of the Employee Required Contribution,
including for cases in which an ALE Member makes available
certain HRA contributions, cafeteria plan contributions, wellness
program incentives, and opt-out payments, see Regulations
sections 1.5000A-3(e)(3)(ii) and 1.36B-2(c)(3)(v)(A). Also see
Notice 2015-87.
Special rules apply for individual coverage HRAs. Generally,
the Employee Required Contribution for the individual coverage
HRA means the required HRA contribution, as defined in
Regulations section 1.36B-2(c)(5)(ii). However, for purposes of
the individual coverage HRA safe harbors in Proposed
Regulations section 54.4980H-5(f), the required contribution is
determined based on the applicable lowest cost silver plan, as
defined in Proposed Regulations 54.4980H-5(f)(7)(iii), and the
Instructions for Forms 1094-C and 1095-C (2023)
-15-

Page 16 of 18 Fileid: … 094c&1095c/2023/a/xml/cycle04/source 9:16 - 26-Sep-2023
The type and rule above prints on all proofs including departmental reproduction proofs. MUST be removed before printing.
monthly premium for the applicable lowest cost silver plan is
determined based on the employee’s age, as defined in
Proposed Regulations 54.4980H(f)(7)(i), and the employee’s
applicable location, as defined in Proposed Regulations
54.4980H(f)(7)(ii).
For an employee offered an individual coverage HRA, the
Employee Required Contribution is the excess of the monthly
premium for the applicable lowest cost silver plan based on the
employee’s applicable age over the monthly individual coverage
HRA amount (generally, the annual individual coverage HRA
amount divided by 12).
Applicable lowest cost silver plan. Generally, the lowest
cost silver plan for an employee for a calendar month is the
lowest cost silver plan for self-only coverage of the employee
offered through the Exchange for the ZIP code of the employee’s
applicable location for the month. If there are different lowest
cost silver plans in different parts of a rating area, an employee’s
applicable lowest cost silver plan is the lowest cost silver plan in
the part of the rating area in which the employee’s applicable
location is located. The lowest cost silver plan for an employee is
the lowest cost silver plan for the lowest age band in the
individual market for the employee’s applicable location. For
more information, see
Employer Lowest Cost Silver Plan
Premium Look-up Table.
Applicable age. For an employee who is or will be eligible for
an individual coverage HRA on the first day of the plan year, the
employee’s applicable age for the plan year is the employee’s
age on the first day of the plan year. For an employee who
becomes eligible during the plan year, the employee’s applicable
age for the remainder of the plan year is the employee’s age on
the date the individual coverage HRA can first become effective
for that employee. Note that for non-calendar year plans or for
employees who become eligible during the plan year, the
applicable age may not be the age reported in Part II of Form
1095-C.
Applicable location. An employee’s applicable location is
where the employee resides for the calendar month, or if the ALE
Member is applying the location safe harbor, the employee’s
primary site of employment for the calendar month.
Employer. For purposes of these instructions, an employer is
the person that is the employer of an employee under the
common-law standard for determining employer–employee
relationships and that is subject to the employer shared
responsibility provisions of section 4980H (these employers are
referred to as ALE Members). For more information on which
employers are ALE Members, see the definitions of Applicable
Large Employer (ALE) and Applicable Large Employer Member
(ALE Member).
Full-time employee. For purposes of Forms 1094-C and
1095-C, the term “full-time employee” means a full-time
employee, as defined under section 4980H and the related
regulations, rather than any other definition of that term that the
ALE Member may use for other purposes. Accordingly, a
full-time employee is an employee who, for a calendar month, is
determined to be a full-time employee under either the monthly
measurement method or the look-back measurement method
(as applicable to that employee). The monthly measurement
method and the look-back measurement method are the two
methods provided under the section 4980H regulations for
determining whether an employee has sufficient hours of service
to be a full-time employee. Under the monthly measurement
method, a full-time employee is an employee who was employed
an average of at least 30 hours of service per week with the ALE
Member during a calendar month. Under the look-back
measurement method, an employee is a full-time employee for
each month of the stability period selected by the ALE Member if
the employee was employed an average of at least 30 hours of
service per week with the ALE Member during the measurement
period preceding that stability period. (The look-back
measurement method for identifying full-time employees is
available only for purposes of determining and computing liability
under section 4980H, and not for purposes of determining if the
employer is an Applicable Large Employer.) For purposes of
both methods, 130 hours of service in a calendar month is
treated as the monthly equivalent of at least 30 hours of service
per week.
An ALE Member must report complete information for all 12
months of the calendar year for any of its employees who were
full-time employees for one or more months of the calendar year.
For more information on the identification of full-time employees,
including discussion of the monthly measurement method and
the look-back measurement method, and the rules for when an
ALE Member may use one or both methods, see Regulations
sections 54.4980H-1(a)(21) and 54.4980H-3, and Notice
2014-49, 2014-41 I.R.B. 66 (describing a proposed approach to
the application of the look-back measurement method in
situations in which the measurement period applicable to an
employee changes).
Note. A former employee (for example, a retiree) is not a
full-time employee for any month after termination of
employment with the ALE Member. However, if the former
employee was a full-time employee for any month of the
calendar year (for example, before retiring mid-year), the ALE
Member must complete information in Part II of Form 1095-C for
all 12 months of the calendar year, using the appropriate codes.
An ALE Member need not file a Form 1095-C for an
individual who for each month of a calendar year is
either not an employee of the ALE Member or is an
employee in a Limited Non-Assessment Period with respect to
section 4980H(b). However, for the months in which the
employee was an employee of the ALE Member, such an
employee would be included in the total employee count
reported on Form 1094-C, Part III, column (c). Also, if during the
Limited Non-Assessment Period the employee enrolled in
coverage under a self-insured, employer-sponsored plan, the
ALE Member must file a Form 1095-C for the employee to report
coverage information for the year.
Full-time equivalent employees. A combination of employees,
each of whom individually is not treated as a full-time employee
because he or she is not employed on average at least 30 hours
of service per week with an employer, but who, in combination,
are counted as the equivalent of a full-time employee solely for
purposes of determining whether the employer is an ALE. For
rules on how to determine full-time equivalent employees, see
Regulations section 54.4980H-2(c).
Governmental Unit and Agency or Instrumentality of a Gov-
ernmental Unit. A Governmental Unit is the government of the
United States, any state or political subdivision thereof, or any
Indian tribal government (as defined in section 7701(a)(40)) or
subdivision of an Indian tribal government (as defined in section
7871(d)). For purposes of these instructions, references to a
Governmental Unit include an Agency or Instrumentality of a
Governmental Unit. Until guidance is issued that defines the
term “Agency or Instrumentality of a Governmental Unit” for
purposes of section 6056, an entity may determine whether it is
an Agency or Instrumentality of a Governmental Unit based on a
reasonable and good faith interpretation of existing rules relating
to agency or instrumentality determinations for other federal tax
purposes.
Health coverage. As used in these instructions, health
coverage refers to minimum essential coverage, unless
otherwise indicated.
Hours of service. An hour of service is each hour for which an
employee is paid, or entitled to payment, for the performance of
TIP
-16-
Instructions for Forms 1094-C and 1095-C (2023)
Page 17 of 18 Fileid: … 094c&1095c/2023/a/xml/cycle04/source 9:16 - 26-Sep-2023
The type and rule above prints on all proofs including departmental reproduction proofs. MUST be removed before printing.
duties for the employer, and each hour for which an employee is
paid, or entitled to payment, for a period of time during which no
duties are performed due to vacation, holiday, illness, incapacity
(including disability), layoff, jury duty, military duty, or leave of
absence. An hour of service does not include any hour of service
performed as a bona fide volunteer of a government entity or
tax-exempt entity, as part of a Federal Work-Study Program (or a
substantially similar program of a state or political subdivision
thereof) or to the extent the compensation for services
performed constitutes income from sources outside the United
States. For additional rules for determining hours of service, see
Regulations sections 54.4980H-1(a)(24) and 54.4980H-3(b),
and Notice 2015-87, Q&A 14, at
IRS.gov/irb/2015-52_IRB/
ar11.html. See section VI of the preamble to the section 4980H
regulations for a discussion of determination of hours of service
for categories of employees for whom the general rules for
determining hours of service may present special difficulties
(including adjunct faculty and commissioned salespeople) and
certain categories of work hours associated with some positions
of employment, including layover hours (for example, for certain
airline employees), on-call hours, and work performed by an
individual who is subject to a vow of poverty as a member of a
religious order.
Individual coverage HRA. An HRA is a type of account-based
health plan that employers can use to reimburse employees for
their medical care expenses. An individual coverage HRA is an
HRA integrated with individual health insurance coverage or
Medicare, subject to certain conditions. For more information
about individual coverage HRAs, see T.D. 9867 and
IRS.gov/
Newsroom/Health-Reimbursement-Arrangements-HRAs.
Limited Non-Assessment Period. A Limited Non-Assessment
Period generally refers to a period during which an ALE Member
will not be subject to an assessable payment under section
4980H(a) and, in certain cases, section 4980H(b), for a full-time
employee, regardless of whether that employee is offered health
coverage during that period.
The first five periods described below are Limited
Non-Assessment Periods with respect to sections 4980H(a) and
4980H(b) only if the employee is offered health coverage by the
first day of the first month following the end of the period. Also,
the first five periods described below are Limited
Non-Assessment Periods for section 4980H(b) only if the health
coverage that is offered at the end of the period provides
minimum value. For more information on Limited
Non-Assessment Periods and the application of section 4980H,
see Regulations section 54.4980H-1(a)(26).
•
First year as ALE period. January through March of the first
calendar year in which an employer is an ALE, but only for an
employee who was not offered health coverage by the employer
at any point during the prior calendar year.
•
Waiting period under the monthly measurement method. If an
ALE Member is using the monthly measurement method to
determine whether an employee is a full-time employee, the
period beginning with the first full calendar month in which the
employee is first otherwise (but for completion of the waiting
period) eligible for an offer of health coverage and ending no
later than 2 full calendar months after the end of that first
calendar month.
•
Waiting period under the look-back measurement method. If
an ALE Member is using the look-back measurement method to
determine whether an employee is a full-time employee and the
employee is reasonably expected to be a full-time employee at
his or her start date, the period beginning on the employee’s
start date and ending not later than the end of the employee’s
third full calendar month of employment.
•
Initial measurement period and associated administrative
period under the look-back measurement method. If an ALE
Member is using the look-back measurement method to
determine whether a new employee is a full-time employee, and
the employee is a variable hour employee, seasonal employee,
or part-time employee, the initial measurement period for that
employee and the administrative period immediately following
the end of that initial measurement period.
•
Period following change in status that occurs during initial
measurement period under the look-back measurement method.
If an ALE Member is using the look-back measurement method
to determine whether a new employee is a full-time employee,
and, as of the employee’s start date, the employee is a variable
hour employee, seasonal employee, or part-time employee, but,
during the initial measurement period, the employee has a
change in employment status such that, if the employee had
begun employment in the new position or status, the employee
would have reasonably been expected to be a full-time
employee, the period beginning on the date of the employee’s
change in employment status and ending not later than the end
of the third full calendar month following the change in
employment status. If the employee is a full-time employee
based on the initial measurement period and the associated
stability period starts sooner than the end of the third full
calendar month following the change in employment status, this
Limited Non-Assessment Period ends on the day before the first
day of that associated stability period.
•
First calendar month of employment. If the employee’s first
day of employment is a day other than the first day of the
calendar month, then the employee’s first calendar month of
employment is a Limited Non-Assessment Period.
Minimum essential coverage (MEC). Although various types
of health coverage may qualify as minimum essential coverage,
for purposes of these instructions, minimum essential coverage
refers to health coverage under an eligible employer-sponsored
plan. An individual coverage HRA is a self-insured group health
plan and an eligible employer sponsored plan. For more details
on minimum essential coverage, see
Minimum essential
coverage in Pub. 974.
Minimum value. A plan provides minimum value if the plan
pays at least 60% of the costs of benefits for a standard
population and provides substantial coverage of in-patient
hospitalization services and physician services. An individual
coverage HRA that is affordable is treated as providing minimum
value.
Offer of health coverage. An ALE Member makes an offer of
coverage to an employee if it provides the employee an effective
opportunity to enroll in the health coverage (or to decline that
coverage) at least once for each plan year. For this purpose, the
plan year must be 12 consecutive months unless a short plan
year of less than 12 consecutive months is permitted for a valid
business purpose. An ALE Member makes an offer of health
coverage to an employee for the plan year if it continues the
employee’s election of coverage from a prior year but provides
the employee an effective opportunity to opt out of the health
coverage. If an ALE Member provides health coverage to an
employee but does not provide the employee an effective
opportunity to decline the coverage, the ALE Member is treated
as having made an offer of health coverage to the employee only
if that health coverage provides minimum value and does not
have an Employee Required Contribution for the coverage for
any calendar month of more than 9.5% (as adjusted) of a
monthly amount determined as the mainland federal poverty line
for a single individual for the applicable calendar year, divided by
12.
For purposes of reporting, an offer to a spouse includes an
offer to a spouse that is subject to one or more reasonable,
objective conditions, regardless of whether the reasonable,
objective conditions are satisfied. For example, an offer of
coverage that is available to a spouse only if the spouse certifies
that the spouse does not have access to health coverage from
Instructions for Forms 1094-C and 1095-C (2023)
-17-
Page 18 of 18 Fileid: … 094c&1095c/2023/a/xml/cycle04/source 9:16 - 26-Sep-2023
The type and rule above prints on all proofs including departmental reproduction proofs. MUST be removed before printing.
another employer is treated as an offer of coverage to the
spouse for reporting purposes. Note that this treatment is for
reporting purposes only, and will generally not affect the
spouse’s eligibility for the premium tax credit if the spouse did
not meet the condition and therefore did not have an actual offer
of coverage. A conditional offer to a spouse is reported by
entering code 1J or 1K (as applicable) on line 14 of Form
1095-C. See the instructions for line 14 for more information. An
offer to a dependent does not include an offer to a dependent
that is subject to one or more reasonable, objective conditions
unless the dependent satisfies the conditions and the dependent
actually had an offer of coverage. In addition, an offer of
coverage is treated as made to an employee’s dependents only
if the offer of coverage is made to an unlimited number of
dependents regardless of the actual number of dependents, if
any, an employee has during any particular calendar month.
An ALE Member offers health coverage for a month only if it
offers health coverage that would provide coverage for every day
of that calendar month. For reporting purposes, this means that
an offer of coverage does not occur for a month if an employee’s
employment terminates before the last day of a calendar month
and the health coverage also ends before the last day of that
calendar month (or for an employee who did not enroll in
coverage, the coverage would have ended if the employee had
enrolled in coverage). However, see the description of Code
Series 2—Section 4980H Safe Harbor Codes and Other Relief
for Employers, code 2B, which may be applicable in these
circumstances to indicate that the ALE Member is treated as
having offered coverage for the entire month for purposes of
section 4980H.
An ALE Member offers health coverage to an employee if it,
or another employer in the Aggregated ALE Group, or a third
party, such as a multiemployer or single employer Taft-Hartley
plan, a multiple employer welfare arrangement (MEWA), or, in
certain cases, a staffing firm, offers health coverage on behalf of
the employer. See Regulations sections 54.4980H-4(b)(2) and
54.4980H-5(b).
Interim Guidance Regarding Multiemployer
Arrangements. An ALE Member is treated as offering
health coverage to an employee if the ALE Member is
required by a collective bargaining agreement or related
participation agreement to make contributions for that employee
to a multiemployer plan that offers, to individuals who satisfy the
plan’s eligibility conditions, health coverage that is affordable and
provides minimum value, and that also offers health coverage to
those individuals’ dependents. For more information, see
section XV.E of the preamble to the final regulations under
section 4980H. This relief is referred to as the “multiemployer
arrangement interim guidance” and the “multiemployer interim
rule relief” in these instructions.
Qualifying Offer. A Qualifying Offer is an offer of MEC
providing minimum value to one or more full-time employees for
TIP
all calendar months during the calendar year for which the
employee was a full-time employee for whom a section 4980H
assessable payment could apply, with an Employee Required
Contribution for each month, not exceeding 9.5 % (as adjusted)
of the mainland single federal poverty line divided by 12,
provided that the offer includes an offer of MEC to the
employee’s spouse and dependents (if any).
Privacy Act and Paperwork Reduction Act Notice. We ask
for the information on these forms to carry out the Internal
Revenue laws of the United States and the Patient Protection
and Affordable Care Act. Our legal right to ask for the information
on this form is Internal Revenue Code sections 6055, 6056,
4980H, and their regulations. We request it to confirm that you
are providing your employees offers of, and enrollment in, health
coverage and to determine the employer shared responsibility
payments and eligibility of your employees for premium tax
credits. If you do not provide this information, we may be unable
to determine whether your employees are entitled to premium
tax credits. Providing false or fraudulent information may subject
you to penalties. We may disclose this information to the
Department of Justice for civil or criminal litigation and to cities,
states, and the District of Columbia for use in administering their
tax laws. We may also disclose this information to other
countries under a tax treaty, to federal and state agencies to
enforce federal nontax criminal laws, or to federal law
enforcement and intelligence agencies to combat terrorism.
You are not required to provide the information requested on
a form that is subject to the Paperwork Reduction Act unless the
form displays a valid OMB control number. Books or records
relating to a form or its instructions must be retained as long as
their contents may become material in the administration of any
Internal Revenue law. Generally, tax returns and return
information are confidential, as required by section 6103.
The time needed to complete and file this form will vary
depending on individual circumstances. The estimated average
time is:
Form 1094-C.................. 4 hr.
Form 1095-C.................. 12 min.
If you have comments concerning the accuracy of these time
estimates or suggestions for making this form simpler, we would
be happy to hear from you. You can send us comments from
IRS.gov/FormComments. Or you can write to the Internal
Revenue Service, Tax Forms and Publications Division, 1111
Constitution Ave. NW, IR-6526, Washington, DC 20224. Don't
send the form to this office.
-18-
Instructions for Forms 1094-C and 1095-C (2023)
