Medical scribes assist health care providers with medical
documentation, thus freeing providers’ time for clinical work.
In 2015, Grand Valley State University (GVSU) partnered with
Helix Scribe Solutions (HSS) to educate medical scribes with
classroom and clinical training, including interprofessional
education (IPE) created by the Midwest Interprofessional
Education and Research Center. This study explored the
impact of an academic scribe training program, including the
effect of IPE on scribe student perceptions of teamwork and
to determine the factor(s) associated with scribe documen-
tation recording accuracy. From August 2016 to October
2018, 196 students consented to participate. Students were
asked to complete the Interprofessional Education Percep-
tion Scale (IEPS) and Entry Level Interprofessional Question-
naire (ELIQ) tools before and after their educational program.
Differences between overall pre- and post-questionnaires
were significant (p<0.05). IEPS subscales, Perception of
Need for Cooperation, Perception of Actual Cooperation,
and Understanding Others’ Values were significant (p<0.05).
The ELIQ subscale Interprofessional Interaction showed sig-
nificant positive scoring (p<0.05). Program evaluations
showed the curriculum prepared the students to work in
emergency department interprofessional teams. Logistic
regression modeling indicated that students’ grade point
average was significant in predicting whether a scribe would
have fewer deficiencies per chart on average as scribe
employees. J Allied Health 2021; 50(4):263–268.
MEDICAL SCRIBES are a major, emerging, new work-
force group in the United States. Medical scribes assist
providers with patient care documentation at the bed-
side, in real-time, and are usually unlicensed allied
health professionals. Emergency Department staff have
used scribes to assist with patient documentation as
early as 1974.
1
The increased digitalization and stan-
dardization of medical records that resulted from the
Affordable Care Act (ACA)
2
has stimulated the growth
of this workforce.
3
With the increased complexity of
electronic health record (EHR) charting, documenta-
tion can occupy as much as 44% of a provider’s time.
4
Clinical environments under pressure for productivity
and efficiency are well suited for the integration of med-
ical scribes.
To meet an increased need and to provide role clarifi-
cation, the Joint Commission defined a scribe as “a
trained medical information professional who special-
izes in charting physician-patient encounters.”
5
Accord-
ing to the Joint Commission, scribes should be trained
on the safe use of EHRs before working in the highly
regulated healthcare environment. A recent federally
funded study reported that properly trained medical
scribes can safely use EHRs and improve documenta-
tion quality.
6
Medical scribes should also be prepared to
work in environments that require interprofessional
teamwork, mutual respect, and open communication.
7
However, the literature is limited on how scribe educa-
tion impacts work performance.
8–11
Scribe education focuses on medical documentation
competency to identify and document key elements of
the history of present illness (HPI), physical exam (PE),
and review of systems (ROS). Most scribes are required
to document a majority of the patient visit which
requires proficient knowledge and practical use of med-
ical terminology, medication information, the patho-
physiology of body systems, coding and billing, labora-
tory definitions and values, and medical equipment,
among others.
With increased emphasis on patient care quality and
safety, providers and policymakers recognize that health-
care workforce shortages necessitate increased collabo-
ration and teamwork across health professions.
12
Uti-
263
INTERPROFESSIONAL EDUCATION
The Impact of Interprofessional Education and Practice
on Medical Scribe Success Working in the Emergency
Department
Jean Nagelkerk, PhD
1
Ryan Cook, MBA
2
Jeff Trytko, MS
1
Lawrence Baer, PhD
3
Joseph Lorenz, MS
1
Emily Callis, MS
4
From
1
Grand Valley State University, Grand Rapids, MI;
2
Helix Scribe
Solutions, Grand Rapids, MI;
3
Independent Contractor, Belmont, MI;
and
4
Eastern Michigan University, Ypsilanti, MI.
The authors report no funding or conflicts of interest related to this
study.
IP2381—Received Mar 26, 2021; accepted June 14, 2021.
Address correspondence to: Mr. Jeff Trytko, College of Health Profes-
sions, Cook-DeVos Center for Health Sciences, Grand Valley State
University, 301 Michigan St. NE, Suite 400, Grand Rapids, MI 49503-
3314, USA. Tel 616-331-2729, fax 616-331-5640. trytkoj@gvsu.edu.
© 2021 Assoc. of Schools Advancing Health Professions, Wash., DC.

lizing interprofessional collaborative practice is essen-
tial to optimally educating the next generation of
healthcare practitioners and improve collaborative
practice.
13
For scribes to work effectively on interpro-
fessional teams, they must learn effective communica-
tion techniques.
Helix Scribe Solutions, a for-profit scribe staffing
company, partnered with Grand Valley State Univer-
sity (GVSU) to create the GVSU Scribe Academy.
Graduates from the Academy become part-time med-
ical scribes through Helix working in emergency depart-
ments. When developing the program, the authors dis-
covered for-profit companies had designed scribe
workforce training and employment programs, but lim-
ited sharing of curricular details.
8–10
GVSU faculty and
staff created the curriculum for the GVSU Scribe Acad-
emy that includes 40 hours of theory and 40 hours of
clinical training. Scribe didactic knowledge is assessed
by passing an examination of the theory portion with a
minimum of 85% to be eligible for clinical training. Cur-
riculum information is located in Appendix 1. As part-
ners of the Midwest Interprofessional Practice, Educa-
tion, and Research Center (MIPERC), elements from
the core IPE content was incorporated into the Acad-
emy curriculum. MIPERC was established in 2007 as an
inter-institutional infrastructure to transform health-
care education and practice.
12–14
Interprofessionl educa-
tion (IPE) was added to the curriculum to smooth the
process for scribe students integrating into the emer-
gency department team. The content includes IPE core
competencies, the scope of practice and professional
role blurring, patient safety, effective communication
behaviors, and team conflict and resolution. The Acad-
emy training is free for all eligible students, with the
agreement to commit to this program and employment
for at least 18 months.
A study was developed to determine the usefulness
of a robust curriculum including IPE content in the
scribe training and to determine factors affecting scribe
student success in the program. The key questions for
the study include: 1) does the inclusion of IPE content
in the medical scribe training curriculum improve per-
ceptions of interprofessional teamwork through clinical
training? and 2) what characteristics from the students’
application materials predict they will be successful
medical scribes?
Methods
This study utilized a quasi-experimental design with the
scribe program as the independent study variable.
Dependent variables were collected from the scribe pro-
gram application and screening materials which
included typing speed, medical terminology test results,
university program major, class level, career and aca-
demic goals, and grade point average (GPA). All pre-
screening was conducted by the GVSU Scribe Director
and support staff. Scribe Academy graduates became
part-time Helix Scribe Solutions employees.
This research was approved by the GVSU Institu-
tional Review Board (IRB study #16-113-H-GVSU).
Students completed an informed consent and demo-
graphic form in addition to application materials prior
to starting the Academy.
Tools and Measures
Students completed the Interdisciplinary Education
Perception Scale (IEPS) and the Entry-level Interprofes-
sional Questionnaire (ELIQ) tools before starting the
Academy and after their clinical rotations. Both assess-
ments were completed online in the learning manage-
ment system Blackboard®, and results were downloaded
to a spreadsheet. The IEPS was tested for validity and
reliability for assessing perceptions of interprofessional
care.
15
This was a tool with 18 items and four subscales:
competency and autonomy (CA), perceived need for
cooperation (PNfC), perception of actual cooperation
(PAC), and understanding others’ values (UOV). The
PNfC subscale addresses perceptions about the collabo-
rative environment.
The ELIQ was used to measure dimensions of team
communications and teamwork and has been tested for
reliability and validity.
16
This tool contains three sub-
scales: communication and teamwork style (CTS),
interprofessional learning (ILS), and interprofessional
interaction (IPIS). Total questions of 27 are divided
evenly into each category utilizing a 5-point Likert-type
scale. This tool categorized scores for each section into
three groups: positive, neutral, and negative. Communi-
cation and style comfort items were included in the
CTS subscale. Respondent’s experience learning with
other health professions was measured in the ILS sub-
scale, and the IPIS included items related to collabora-
tive practice perceptions and communication among
health professions.
Scribes completed a program evaluation at the end
of clinical training that included narrative questions
about the course and working on the interprofessional
emergency department team; as an example one ques-
tion asked, “What efficiencies are gained in the emer-
gency department by having a scribe work with a
provider?” Students were asked to complete this by the
program director upon the decision of their pass/fail of
the clinical training.
Scribe success was measured through standardized
charts drafted by Helix scribe employees. Standard
monthly chart audits were conducted. A selection of 12
charts per month per scribe were audited by a team of
experienced full-time Helix scribes. Charts were evalu-
ated on three criteria including accuracy, narrative flow,
and spelling and grammar. The numbers of deficiencies
per chart were tracked and averaged on a central
spreadsheet maintained by Helix leadership.
264
NAGELKERK ET AL., IPE and Medical Scribe Success in the ED
Data Analysis
Demographic data were summarized with descriptive
statistics. The sample size, normality, and symmetry of
differences were assessed to determine appropriate sta-
tistical analysis.
The direct effect on scribe student interprofessional
attitudes was tested by comparison of results from
instruments completed at baseline to those completed
at the end of clinical training. Two assessments were uti-
lized for this: IEPS and ELIQ. Changes in relevant
knowledge and perception were tested with paired t-
tests. This included the examination of four factors
measured with IEPS. The ELIQ instrument grouped its
underlying ordinal scale into three ordinal categories
and so Wilcoxon matched-pairs signed rank was used.
Qualitative data from program evaluation surveys
were used to examine emerging themes. The author
team reviewed the results and coded responses based on
common themes that emerged. The consensus was
established by three of the authors. Binary logistic
regression was used to look at what factors were signifi-
cant in predicting scribe success. The outcome variable
of interest for this model was defined as whether the
student had 4 consecutive months with an average of
three or fewer deficiencies per chart audit. This process
is proprietary to Helix Scribe Solutions per lack of
available resources in the literature. All factors were put
into the model utilizing a backward method, where the
variable with the highest p-value was removed, until
only significant variables remained. Data analysis was
performed using SAS Enterprise Guide 7.1 software.
Significance for all tests was set at p<0.05.
Results
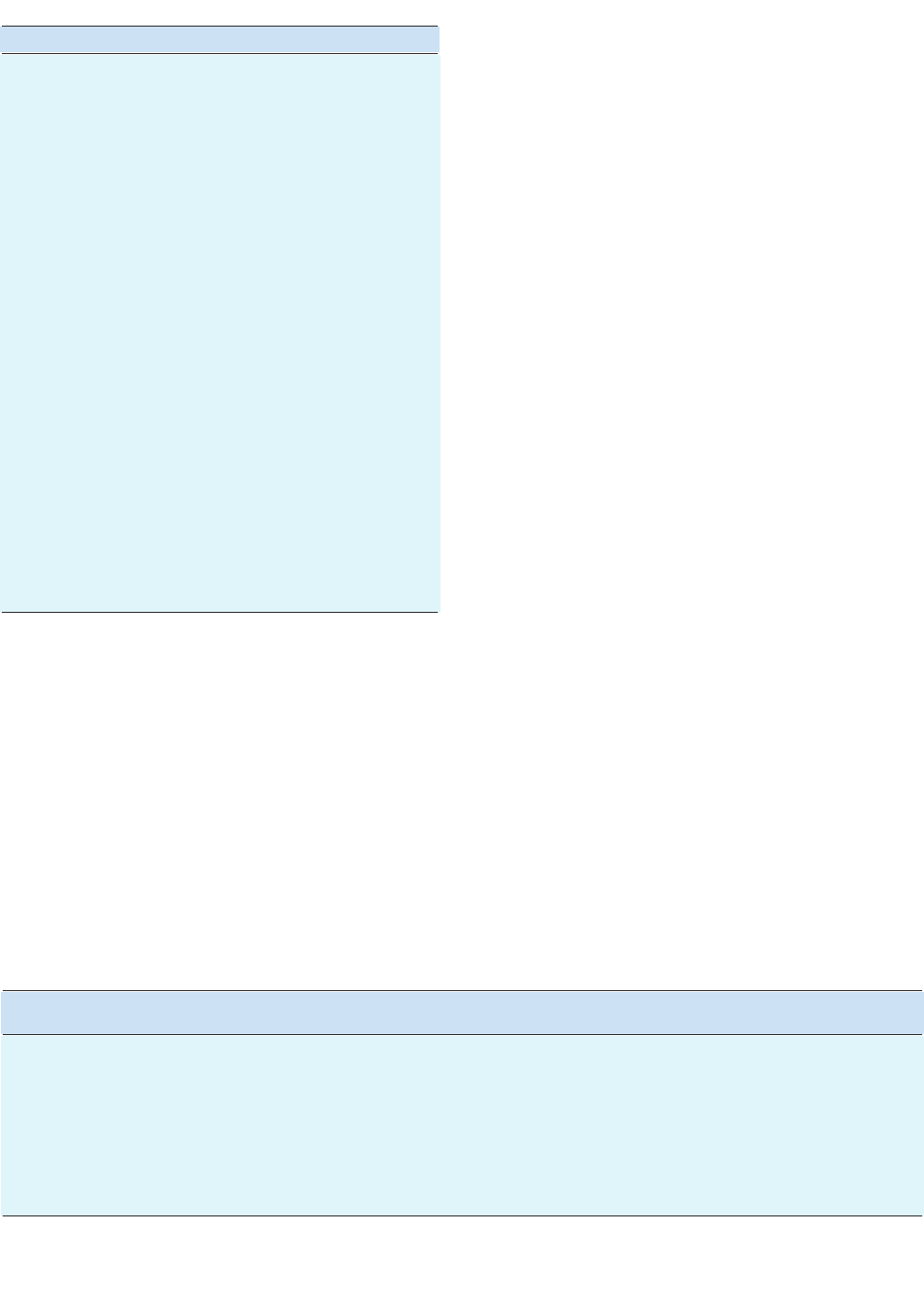
Description of study participants (n=194, Table 1) shows
that 66.3% of participants were female, and most had
not had IPE in the past.
The overall IEPS scores were positive when compared
to baseline values and demonstrated significant (p<0.05)
improvement. Table 2 shows the four measures also
tested within IEPS. All but the competency and auton-
omy subscales were considered significant. The overall
ELIQ and subscale average scores were in the positive
range and were determined to show improved perception
of interprofessional knowledge (p=0.012, Table 2).
The scribe students completed the program evalua-
tions after 40 hours of clinical training working with
emergency department providers as a team. From the
102 respondents, three themes emerged: 1) focus on
patient care; 2) increased throughput; and 3) decreased
workload (Table 3).
The factors entered into the logistic regression
model and results are listed in Table 4: medical termi-
nology pretest score, whether or not they had prior
Journal of Allied Health, Winter 2021, Vol 50, No 4
265
TABLE 1. Study Participants (n=174)
Characteristics No. (%)
Gender
Male 56 (31.5)
Female 118 (66.3)
Missing 4 (2.2)
Race
Asian 21 (11.8)
Black or African American 6 (3.4)
Caucasian 137 (77)
Multiracial 7 (3.9)
Other 1 (0.6)
Missing 6 (3.4)
Ethnicity
Hispanic 6 (3.4)
Non-Hispanic 167 (93.8)
Missing 5 (2.8)
Education highest degree obtained
High school (enrolled in 4-yr college) 105 (59)
Associate degree/certicate/diploma 27 (15.2)
Baccalaureate degree 33 (18.5)
Master’s degree 2 (1.1)
Missing 11 (6.2)
Prior interprofessional course
Ye s 11 (6.2)
No 162 (91 )
Missing 5 (2.8)
Prior interprofessional education
Ye s 5 (2.8)
No 168 (94.4)
Missing 5 (2.8)
TABLE 2. IEPS and ELIQ Testing Results
Pre vs Post Test
Average Difference SD p-Value
Interprofessional Education Scale (IEPS) (n=119) 3.24 11.15 0.002*
Competency and autonomy 0.96 6.09 0.089
Perception of need for cooperation 0.35 1.63 0.020*
Perception of actual cooperation 1.32 3.71 <0.001*
Understanding others value 0.61 2.34 0.006*
Entry-Level Interprofessional Questionnaire (ELIQ) (n=92) 2.37 8.88 0.012*
Communication and teamwork –1.11 2.73 <0.001*
Interprofessional learning –1.02 4.11 0.019*
Interprofessional interaction 2.39 6.26 <0.001*
* ≤ 0.05.
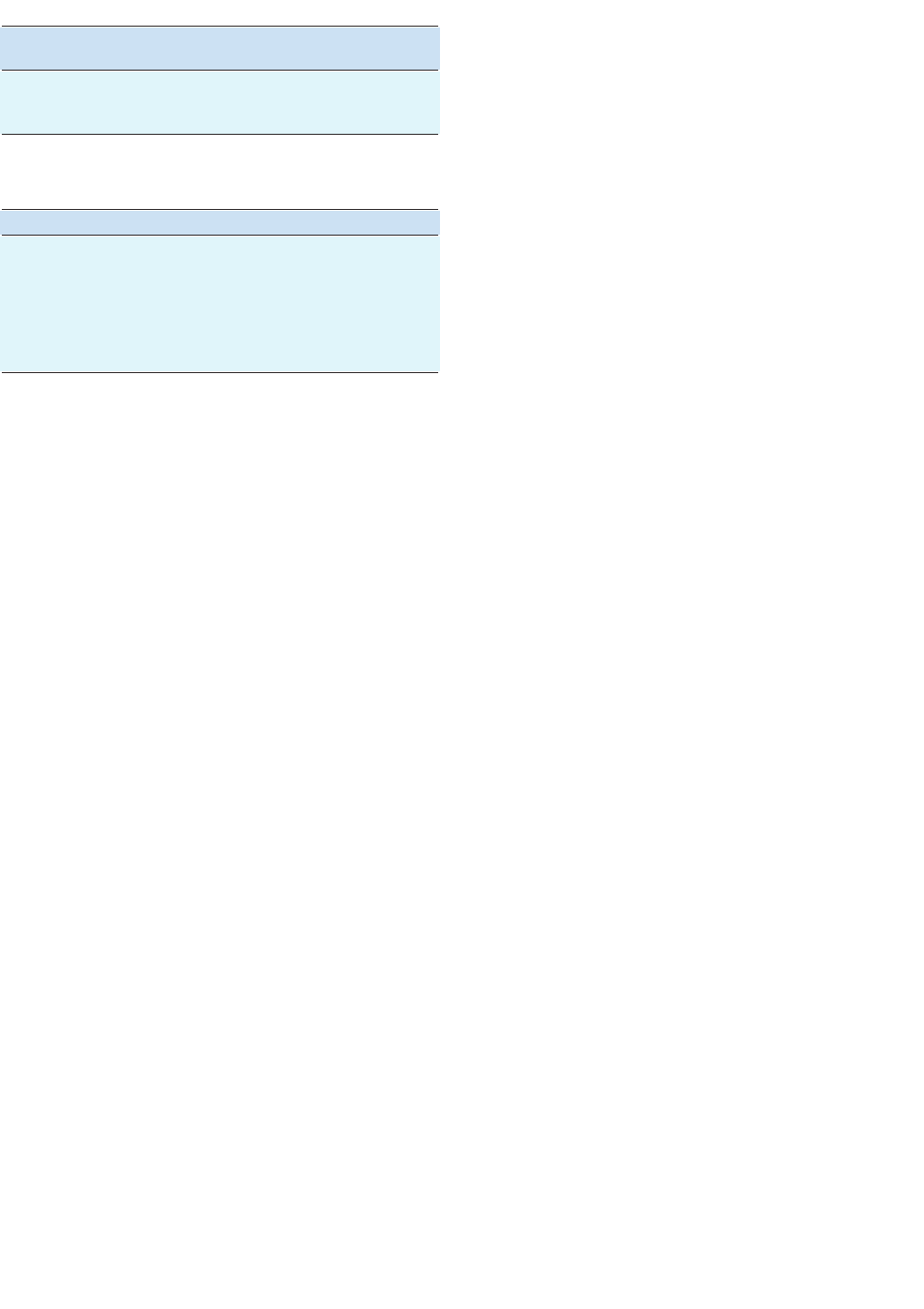
clinical experience, university program major, level of
credit earned, last degree earned, typing speed, and
GPA. Six of the seven factors were considered insignifi-
cant with a cutoff value of p>0.05. GPA was considered
a significant factor in predicting whether a GVSU
Scribe Academy graduate will have three or fewer defi-
ciencies per chart on average over 4 consecutive
months as an employed scribe.
Discussion
Scribe students’ perceptions of interprofessional educa-
tion and practice improved from baseline to the com-
pletion of the Academy. Most students had no prior
IPE and reported positive perceptions of collaborative
care in their program evaluations, which is similar to
research results in the literature.
17,18
All of the subscales
showed statistical improvement except for an improve-
ment in perceived autonomy. This may be attributed to
the scribes’ scope of practice as allied health profession-
als who are not directly responsible for patient care
decisions (the Joint Commission).
We examined the characteristics of effective scribe
students working on the emergency department team
based on the quality of scribe health records. Of the fac-
tors we evaluated for successful students during the
screening process, GPA showed to be the only signifi-
cant. Higher GPAs may indicate a student’s work ethic
and desire to perform well. Other authors describing
their scribe models did not find having a college back-
ground necessary, yet also stated that scribes experience
a steep learning curve for completing more complex
medical documentation.
9
We found students already
enrolled in a higher education program with at least
two semesters as full-time students are better prepared
with the study habits to be successful in a higher-educa-
tion-based scribe training program.
The literature shows scribe programs best prepare stu-
dents to adapt to providers by including clinical training
in the curriculum. An important aspect of the Academy
was the 40 hours of clinical training that prepared the
scribes to put the Academy theory training and IPE into
practice by “follow in the footsteps” of providers without
stepping on their toes.
10
Yan et al.
10
observed that
provider and scribe teamwork is achieved through a trial
process during shifts. The scribes in Yan et al.’s paper
started scribing after having achieved certification in
another health profession, contrasting with our students
who did not have extensive prior clinical experiences.
10
Our data show the GVSU Scribe Academy curriculum
including IPE laid the foundation for a smooth transi-
tion for building the provider and scribe team.
The GVSU Scribe Academy program evaluations
provided rich data with three themes emerging from
scribe student responses (Table 3). The first theme
related to the student’s satisfaction with their contribu-
tion to assisting providers to focus more on patient
care. They reported how their role through documenta-
tion helped the providers to have uninterrupted face-to-
face time with patients and time for medical decision-
making and coordination of treatment plans. This
study did not evaluate how the scribes helped the
providers specifically, but other studies observed that
scribes assist providers by adapting to their workflow.
11
The physician takes the lead, and the scribe conforms
to their work habits to better fit the provider’s.
Providers also learn how to adapt their work for the
scribe to be a more effective teammate, e.g., verbalizing
physical exam findings in the room.
9,11
The second theme that emerged was the scribe’s
observation of provider patient care throughput
enhanced by the delegation of patient documentation.
This paper’s authors received feedback from providers
on how GVSU Scribe Academy graduates help them
with efficiency and writing high-quality, detailed, med-
ical notes.
19
A PubMed search for “medical scribes” in
April 2020 showed over 35 peer-reviewed papers report-
ing improved provider productivity through patients
seen per shift, decreased time spent for providers docu-
menting, and increases in relative value units. Increased
productivity with a medical scribe assists with more
accurate notes for improved reimbursements leading to
increased revenue.
20–23
The scribe’s contributions to
provider improved throughput can offset the added cost
for scribe training programs and staffing.
24,25
Finally, scribes reported observing a decrease in cleri-
cal workload on providers, allowing them time to focus
more on patient management. One provider told the
authors that having a scribe allows them to focus more
on the clinical needs for the patient, so they can focus
more on the patient’s problem, history, physical exam,
and treatment plan.
18
This is consistent with other stud-
266
NAGELKERK ET AL., IPE and Medical Scribe Success in the ED
TABLE 3. Student Program Evaluation Results
What efciencies are gained in the ED
by having a scribe work with a provider? (n=102) No. (%)
Providers can focus more on patient care 45 (44.1)
Increased patient throughput 38 (37.3)
Decreased workload for providers 19 (18.6)
ED, emergency department.
TABLE 4. Output of Logistic Regression Analysis
Predictor Variable Wald Chi-Squared p-Value
Pretest 0.2221 0.638
Clinical experience 0.8485 0.357
Major 1.2414 0.265
Level of credits earned 2.6475 0.104
Last earned degree 1.9521 0.162
Typing speed 1.8948 0.169
Grade point average* 11.6090 <0.001†
* Estimate = 2.0002. † = 0.05

ies that have reported scribes decreased the time
providers spent documenting in electronic medical
records by 50%.
7,26
Not only do scribes assist with efficien-
cies in patient care flow, but they also aided providers
during clinical shifts to have more time teaching resi-
dents, increasing the quality of their education.
27,28
With
a greater focus on patient-related tasks, this has been
shown to increase provider satisfaction.
29–32
Decreasing
the documentation workload on providers is one solu-
tion to provider burnout.
33,34
Limitations
This study investigated various aspects of a single scribe
program. Our findings may not reflect the “advanced
‘dual-trained’ scribes” who not only focus on medical
documentation but also close care gaps other health
professions can delegate, such as rooming patients and
motivational interviewing.
33,35
At the inception of the
GVSU Scribe Academy, the eligibility criteria were
established to ensure student success. These results do
not reflect the medical scribe workforce not sharing
these same criteria. Additionally, qualitative data could
not be collected from providers to further explore the
benefits of scribing and the role of the scribe as an inter-
professional care team member. Lastly, the lack of an
accrediting body to standardize criteria for professional
certification makes it difficult to compare scribe pro-
gram curriculum and quality.
Conclusion
The GVSU Scribe Academy was created to assist emer-
gency medicine providers in meeting the growing
demands of medical record documentation. Scribes are
not licensed health professionals and are unable to per-
form patient care tasks, though they contribute to pro-
vider efficiencies by improving medical documentation
and throughput and by enabling increased workload.
Including IPE in the academic core scribe curriculum
had aided students naïve to the healthcare environ-
ment through clinical training and into employment.
Scribe perceptions of providers and teamwork
improved on both the IEPS and ELIQ subscales. The
most successful scribes were those with high GPAs. Fur-
ther exploration is needed on the provider’s percep-
tions of scribe interprofessional competencies and
teamwork characteristics. National standardization of
scribe education would be helpful to ensure the quality
of the scribe workforce.
References
1. Lynch TS. An emergency department scribe system. J Am Coll
Emerg Physicians. 1974 Sep;3(5):302–3.
2. Patient Protection Affordable Care Act. 42 U.S.C, 18001 2010.
3. Bossen C, Chen Y, Pine KH. The emergence of new data work
occupations in healthcare: the case of medical scribes. Int J Med
Inform. 2019 Mar;123:76–83.
4. Hess J, Wallenstein J, Ackerman J, et al. Scribe impacts on
provider experience, operations, and teaching in an academic
emergency medicine practice. West J Emerg Med. 2015 Sep
15;16(5):602–10.
5. The Joint Commission. Standard FAQs: Documentation Assis-
tance Provided By Scribes. Updated 2020 Apr 16. Available
from: https://www.jointcommission.org/standards/standard-
faqs/ambulatory/record-of-care-treatment-and-services-
rc/000002210/ [cited 2020 Aug 12].
6. Ash JS, Corby S, Mohan V, et al. Safe use of the EHR by medical
scribes: a qualitative study. J Am Med Inform Assoc. 2020 Oct 29.
https://doi.org/10.1093/jamia/ocaa199
7. Imdieke BH, Martel ML. Integration of medical scribes in the
primary care setting: improving satisfaction. J Ambul Care
Manage. 2017;40(1):17–25.
8. Baugh R, Jones JE, Trott K, et al. Medical scribes. J Med Pract
Manage. 2012 Dec;28(3):195–7.
9. Gellert GA, Ramirez R, Webster SL. The rise of the medical
scribe industry: implications for the advancement of electronic
health records. JAMA. 2015 Apr 7;313(13):1315.
10. Yan C, Rose S, Rothberg MB, et al. Physician, scribe, and patient
perspectives on clinical scribes in primary care. J Gen Intern Med.
2016 Sep;31(9):990–5.
11. Addesso LC, Nimmer M, Visotcky A, et al. Impact of medical
scribes on provider efficiency in the pediatric emergency depart-
ment. Acad Emerg Med. 2018 Oct 23. https://onlinelibrary.
wiley.com/doi/abs/10.1111/acem.13544
12. Interprofessional Education Collaborative Expert Panel. Core
Competencies for Interprofessional Collaborative Practice: 2016
update [Internet]. Washington, DC: IPEC; 2016. Available from:
https://hsc.unm.edu/ipe/resources/ipec-2016-core-competen-
cies.pdf
13. Reeves S, Perrier L, Goldman J, et al. Interprofessional educa-
tion: effects on professional practice and healthcare outcomes
(update). Cochrane Datab Syst Rev. 2013. http://doi.wiley.
com/10.1002/14651858.CD002213.pub3
14. Nagelkerk J, Coggan P, Pawl B, Thompson ME. The Midwest
Interprofessional Practice, Education, and Research Center: a
regional approach to innovations in interprofessional education
and practice. J Interprof Educ Pract. 2017 Jun;7:47–52.
15. Luecht R, Madsen M, Taugher M, Petterson B. Assessing profes-
sional perceptions: design and validation of an interdisciplinary
education perception scale. J Allied Health. 1990 Spring;19(2):
181–91.
16. Pollard KC, Miers ME, Gilchrist M. Collaborative learning for
collaborative working? Initial findings from a longitudinal study
of health and social care students. Health Soc Care Community.
2004 Jul 1;12(4):346–58.
17. Kururi N, Makino T, Kazama H, et al. Repeated cross-sectional
study of the longitudinal changes in attitudes toward interpro-
fessional health care teams amongst undergraduate students. J
Interprof Care. 2014 Jul;28(4):285–91.
18. Nagelkerk J, Thompson ME, Bouthillier M, et al. Improving out-
comes in adults with diabetes through an interprofessional col-
laborative practice program. J Interprof Care. 2017 Nov 7;1–10.
19. Helix Scribe Solutions. [cited 2020 Aug 12]. Available from:
https://www.helixscribes.com/Core/Gallery/Spotlights/1000/
20. Dawkins B, Bhagudas KN, Hurwitz J, et al. An analysis of physi-
cian productivity and self-sustaining revenue generation in a
free-standing emergency department medical scribe model. Adv
Emerg Med. 2015;2015:1–9.
21. Bank AJ, Gage RM. Annual impact of scribes on physician pro-
ductivity and revenue in a cardiology clinic. Clinicoecon Out-
comes Res. 2015;7:489–95.
22. Earls ST, Savageau JA, Begley S, et al. Can scribes boost FPs’ effi-
Journal of Allied Health, Winter 2021, Vol 50, No 4
267
ciency and job satisfaction? J Fam Pract. 2017 Apr;66(4):206–14.
23. Zallman L, Finnegan K, Roll D, et al. Impact of medical scribes
in primary care on productivity, face-to-face time, and patient
comfort. J Am Board Fam Med. 2018 Jul;31(4):612–9.
24. Hegstrom L, Leslie J, Hutchinson E, et al. 560: medical scribes:
are scribe programs cost effective in an outpatient MFM setting?
Am J Obstet Gynecol. 2013 Jan;208(1):S240.
25. Walker K, Ben-Meir M, Dunlop W, et al. Impact of scribes on
emergency medicine doctors’ productivity and patient through-
put: multicentre randomised trial. BMJ. 2019 Jan 30;l121.
26. Taylor KA, McQuilkin D, Hughes RG. Medical scribe impact on
patient and provider experience. Milit Med. 2019 Feb 27. Avail-
able from: https://academic.oup.com/milmed/advance-arti-
cle/doi/10.1093/milmed/usz030/5366283
27. Delage BS, Sherman K, Halaas G, Johnson EL. Getting the
predoc back into documentation: students as scribes during
their clerkship. Fam Med. 2020 Apr 3;52(4):291–4.
28. Wegg B, Deibel M, Kiernan C. 162 advancing resident training
with the use of scribes. Ann Emerg Med. 2014 Oct;64(4):S59.
29. Koshy S, Feustel PJ, Hong M, Kogan BA. Scribes in an ambula-
tory urology practice: patient and physician satisfaction. J Urol.
2010 Jul;184(1):258–62.
30. Bastani A, Shaqiri B, Palomba K, et al. An ED scribe program is
able to improve throughput time and patient satisfaction. Am J
Emerg Med. 2014 May;32(5):399–402.
31. Gidwani R, Nguyen C, Kofoed A, et al. Impact of scribes on
physician satisfaction, patient satisfaction, and charting effi-
ciency: a randomized controlled trial. Ann Fam Med. 2017
Sep;15(5):427–33.
32. Sattler A, Rydel T, Nguyen C, Lin S. One year of family physi-
cians’ observations on working with medical scribes. J Am Board
Fam Med. 2018 Jan;31(1):49–56.
33. Reick-Mitrisin V, MacDonald M, Lin S, Hong S. Scribe impacts
on US health care: benefits may go beyond cost efficiency. J
Allerg Clin Immunol. 2020 Feb;145(2):479–80.
34. Yates SW. Physician Stress and Burnout. Am J Med. 2020 Feb;
133(2):160–4.
35. Martel ML, Imdieke BH, Holm KM, et al. Developing a medical
scribe program at an academic hospital: the Hennepin County
Medical Center experience. Joint Comm J Qual Patient Saf. 2018
May;44(5):238–49.
Published online 1 Dec 2021
www.ingentaconnect.com/content/asahp/jah
© 2021 ASAHP, Washington, DC.
268
NAGELKERK ET AL., IPE and Medical Scribe Success in the ED
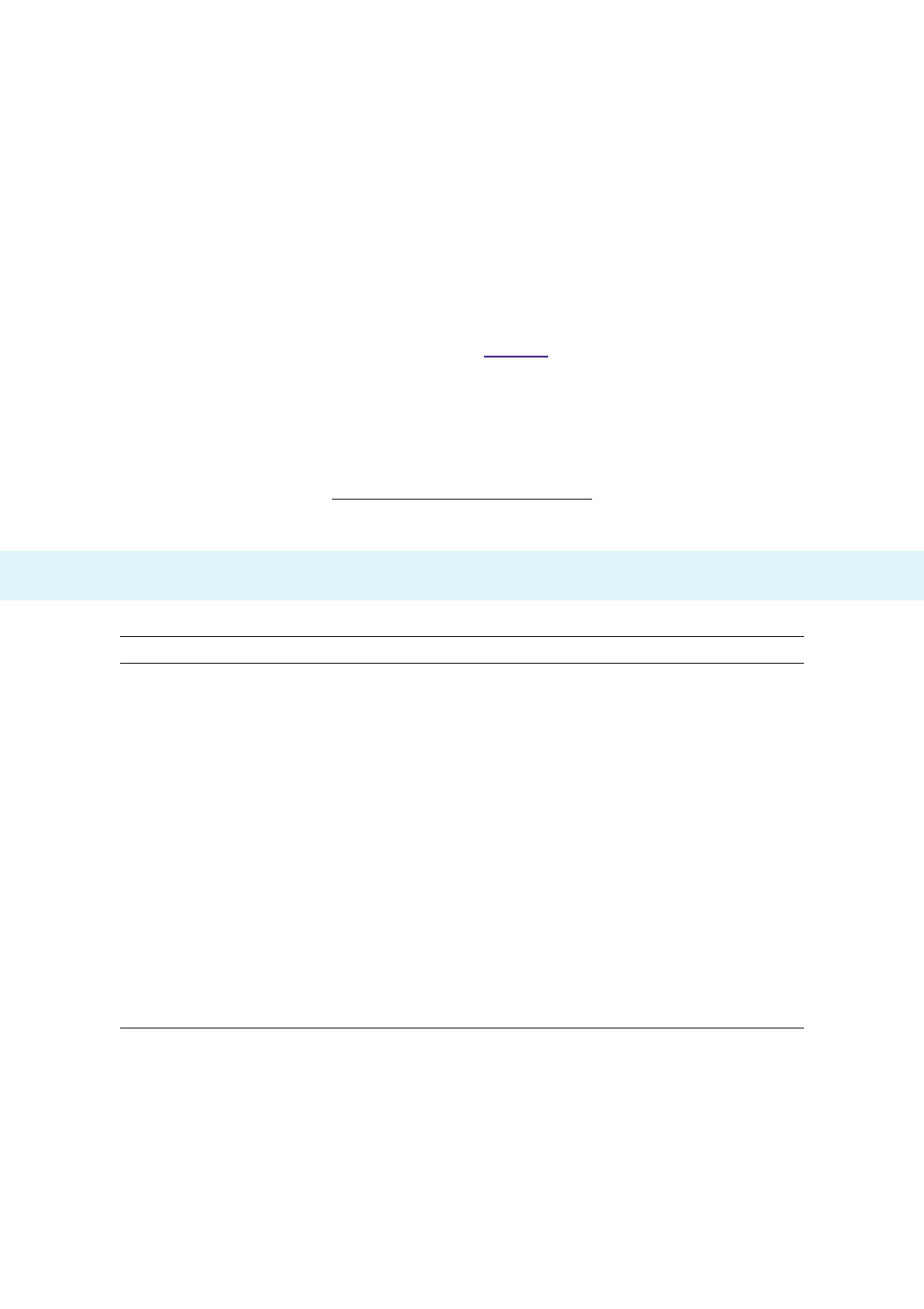
Content Format Hours
Scribe academy kickoff - orientation Online 2
GVSU HIPAA & BBP training modules Online 2
Common ED medications Online 2
Joint Commission Online 1
What is a medical scribe? (professional role identity) Online 0.5
Introduction to the history of present illness note Online 0.5
Common ED procedures and equipment Online 2
ED radiology imaging Online 1
Laboratory tests Online 1
Physical exam and review of systems Online 3
Basics of the medical note Online 4
Basics of medical coding and billing Online 4
Body systems/pathophysiology Online 8
Interprofessional education Online 1
Introduction to electronic medical record and charting simulation In-person 3
Charting simulation, introduction to clinical training and ED In-person 4
Comprehensive nal exam Online 1
Clinical training (5 shifts) Clinical 40
Total 80
ED, emergency department.
APPENDIX 1. GVSU Scribe Academy Curriculum
