
UIN: NIAHLIP24123V032324 Page 1 of 24
NEW INDIA ASHA KIRAN POLICY
THE NEW INDIA ASSURANCE CO. LTD.
REGISTERED & HEAD OFFICE: 87, MAHATMA GANDHI ROAD, MUMBAI 400001
NEW INDIA ASHA KIRAN POLICY- PROSPECTUS
We welcome You as Our Customer. This document explains how the NEW INDIA ASHA KIRAN POLICY
could provide value to You. In the document the word ‘You’, ‘Your’ means the all the members covered
under the Policy. ‘We’, ‘Our’, ‘Us’ means The New India Assurance Co. Ltd.
New India Asha Kiran is a Policy designed to cover Hospitalisation expenses of the family and Personal
Accident for Parents.
1. WHO CAN TAKE THIS POLICY?
THIS POLICY IS DESIGNED TO THE PARENTS WITH ONLY GIRL CHILDREN. This insurance is available to
persons between the age of 18 years and 65 years. Daughter(s) from 3 months up to 25 years can be
covered provided they are financially dependent on the parents and one or both parents are covered
simultaneously. The upper age limit will not apply to mentally challenged daughter(s) and unmarried
dependent daughter(s). The persons beyond 65 years can continue their insurance provided they are
insured under the Policy with us without any break
Midterm inclusion is allowed for Newly Born Daughter (after completing 3 months) by charging pro-rata
Premium for the remaining period of the Policy.
2. CAN I COVER MY FAMILY MEMBERS IN ONE POLICY?
Yes. You can cover the entire family under a Single Sum Insured (Floater). The members of the family who
could be covered under the Policy are:
a) Proposer
b) Proposer’s Spouse
c) Proposer’s Dependent Daughter (Maximum Two)
Minimum two members, with at least one daughter, are required in this policy. This policy cannot be given
to a single person. Maximum four members can be covered in a single policy. Midterm inclusion is allowed
only for new born 2nd baby girl child on payment of pro - rata additional premium.
3. WHAT DOES THE POLICY COVER?
This Policy is designed to give You and Your family, protection against unforeseen Hospitalization expenses
and Accident cover to Proposer and Spouse.
4. WHAT ARE THE EXPENSES COVERED UNDER THIS POLCY?
Our liability for all claims admitted during the Period of Insurance in respect of all Insured Persons
shall not exceed the Sum Insured. Subject to this, for each claim We will reimburse the following
UIN: NIAHLIP24123V032324 Page 2 of 24
NEW INDIA ASHA KIRAN POLICY
Reasonable and Customary and Medically Necessary Expenses admissible as per the terms and
conditions of the Policy:
(a)
Room rent, Boarding, DMO / RMO / CMO / RMP Charges, Nursing (Including Injection /
Drugs and Intra venous fluid administration expenses), not exceeding 1% of the Sum
Insured per day.
(b)
Intensive Care Unit (ICU) / Intensive Cardiac Care Unit (ICCU), Intensivist charges, Monitor
and Pulse Oxymeter expenses, not exceeding 2% of the Sum Insured per day.
(c)
Associate Medical Expenses; such as Professional fees of Surgeon, Anaesthetist,
Consultant, Specialist; Anaesthesia, Operating Theatre Charges and Procedure Charges
such as Dialysis, Chemotherapy, Radiotherapy & similar medical expenses related to the
treatment.
(d)
Cost of Pharmacy and Consumables, Cost of Implants and Medical Devices and Cost of
Diagnostics.
(e)
Pre-Hospitalization Medical Expenses, not exceeding thirty days
(f)
Post-Hospitalization Medical Expenses, not exceeding sixty days
(g)
Proportionate Deduction is applicable on the Associate Medical Expenses, if the Insured
Person opts for a higher Room than his eligible category. It shall be effected in the same
proportion as the eligible rate per day bears to the actual rate per day of Room Rent.
However, it is not applicable on
1. Cost of Pharmacy and Consumables
2. Cost of Implants and Medical Devices
3. Cost of Diagnostics.
Proportionate Deduction shall also not be applied in respect of Hospitals which do not
follow differential billing or for those expenses in which differential billing is not adopted
based on the room category, as evidenced by the Hospital’s schedule of charges / tariff.
Note:
(h) MEDICAL EXPENSES INCURRED UNDER TWO POLICY PERIODS:
If the claim event falls within two policy periods, the claims shall be paid taking into
consideration the available Sum Insured of the expiring Policy only. Sum Insured of the
Renewed Policy will not be available for the Hospitalisation (including Pre & Post Hospitalisation
Expenses), which has commenced in the expiring Policy. Claim shall be settled on per event
basis.
(i) MEDICAL EXPENSES FOR ORGAN TRANSPLANT:
If treatment involves Organ Transplant to Insured Person, then We will also pay Hospitalisation
Expenses (excluding cost of organ) incurred on the donor, provided Our liability towards
expenses incurred on the donor and the insured recipient shall not exceed the aggregate of the
Sum Insured, if any, of the Insured Person receiving the organ.
UIN: NIAHLIP24123V032324 Page 3 of 24
NEW INDIA ASHA KIRAN POLICY
(j) Dental Treatment (Inpatient): We will cover for medical expenses incurred towards dental
treatment done under anaesthesia necessitated due to an accident/injury/illness requiring
Hospitalization as Inpatient treatment.
LIMIT ON PAYMENT FOR CATARACT
Our liability for payment of any claim within the Period of Insurance, relating to Cataract for
each eye shall not exceed 10% of the Sum Insured or Rs. 50,000, whichever is less.
TREATMENTS UNDER AYURVEDIC/HOMEOPATHIC/UNANI SYSTEMS
Our liability for expenses incurred for Ayurvedic/Homeopathic/Unani treatments shall not
exceed 25% of the Sum Insured in respect of all such treatments admitted during the Period
of Insurance, provided the treatment for Illness or Injury, is taken in any AYUSH Hospital.
HOSPITAL CASH
We will pay Hospital Cash at the rate of 0.1% of the Sum Insured, for each day of Hospitalisation,
admissible under the Policy. The payment under this Clause for Any One Illness shall not exceed
1% of the Sum Insured. The payment under this Clause is applicable only where the period of
Hospitalization exceeds twenty-four hours.
CRITICAL CARE BENEFIT
If during the Period of Insurance any Insured Person discovers that he or she is suffering from
any Critical Illnesses as defined under 2.8 of the Policy Clause, which results in a claim admissible
under this Policy, 10% of the Sum Insured would be paid as Critical Care Benefit along with the
admissible claim amount.
Critical Care Benefit is payable only once in the life time of each Insured Person and is not
applicable to any Insured Persons for whom it is a Pre- Existing Condition/Disease.
Any payment under this Clause would be in addition to the Sum Insured and shall not deplete
the Sum Insured.
PAYMENT OF AMBULANCE CHARGES
We will pay You the charges for Ambulance services not exceeding 1% of the Sum Insured per
Insured event, Medically Necessarily incurred for shifting any Insured Person to Hospital for
admission in Emergency Ward or ICU, or from one Hospital to another Hospital for better
medical facilities.
PAYMENTS ONLY IF INCLUDED IN HOSPITAL BILL
No payment shall be made for any Hospitalisation expenses incurred, unless they form part of
the Hospital Bill. However, the bills raised by Surgeon, Anaesthetist directly and not included in
the Hospital Bill shall be paid provided a numbered Bill is produced in support thereof, for an

UIN: NIAHLIP24123V032324 Page 4 of 24
NEW INDIA ASHA KIRAN POLICY
amount not exceeding Rs. Ten thousand, where such payment is made in cash and for an
amount not exceeding Rs. Twenty thousand, where such payment is made by cheque.
TREATMENT FOR CONGENITAL DISEASES
Congenital Internal Disease or Defects or anomalies shall be covered after twenty-four months
of Continuous Coverage. if it was unknown to You or to the Insured Person at the
commencement of such Continuous Coverage. Exclusion for Congenital Internal Disease or
Defects or Anomalies would not apply to a New Born Baby during the year of Birth and also
subsequent renewals, if Premium is paid for such New Born Baby and the renewals are effected
before or within thirty days of expiry of the Policy.
Congenital External Disease or Defects or anomalies shall be covered after forty-eight months
of Continuous Coverage, but such cover for Congenital External Disease or Defects or anomalies
shall be limited to 10% of the average Sum Insured in the preceding four years.
OPTIONAL COVER I: NO PROPORTIONATE DEDUCTION
On payment of additional Premium as mentioned in Schedule, it is hereby agreed and declared
that Clause 3.1(g) stands deleted for the members covered in the Policy as stated in the
Schedule.
You shall continue to bear the differential between actual and eligible Room Rent.
OPTIONAL COVER II: MATERNITY EXPENSES BENEFIT
On the payment of additional Premium as mentioned in Schedule, it is hereby agreed and
declared that Clause 4.4.15 stands deleted for Insured Person as mentioned in the Schedule.
Our liability for claim admitted for Maternity shall not exceed 10% of the average Sum Insured
of the Insured Person in the preceding three years. This Optional Cover is available for Sum
Insured 5 L & above.
Special conditions applicable to Maternity Expenses Benefit:
i These Benefits are admissible only if the expenses are incurred in Hospital as inpatients in
India.
ii A waiting period of thirty-six months is applicable, from the date of opting this cover, for
payment of any claim relating to normal delivery or caesarian section or abdominal
operation for extra uterine pregnancy. The waiting period may be relaxed only in case of
miscarriage or abortion induced by accident or other medical emergency.
iii Claim in respect of delivery for only first two children and / or surgeries associated
therewith will be considered in respect of any one Insured Person covered under the
Policy or any renewal thereof.
iv Expenses incurred in connection with voluntary medical termination of pregnancy during
the first 12 weeks from the date of conception are not covered.

UIN: NIAHLIP24123V032324 Page 5 of 24
NEW INDIA ASHA KIRAN POLICY
Pre-natal and post-natal expenses are not covered unless admitted in Hospital and treatment
is taken there.
OPTIONAL COVER III: REVISION IN LIMIT OF CATARACT
This optional cover, if opted, will be in addition to limit specified in Clause 3.2 of the Policy
Clause. This Optional Cover is available for Sum Insured 8 L & above.
On payment of additional Premium as mentioned in Schedule, it is declared and agreed that
following additional amount for Cataract shall become payable but not exceeding the actual
expenses incurred:
Sum Insured
Additional Cataract limit
Rs. 8,00,000
Rs. 80,000
Rs. 10,00,000
Rs. 1,00,000
Rs. 12,00,000
Rs. 1,20,000
Rs. 15,00,000
Rs. 1,50,000
Note: Benefit of this cover will be available after the expiry of thirty-six months from the date
of opting this cover.
OPTIONAL COVER IV: NON-MEDICAL ITEMS (CONSUMABLES)
On payment of additional Premium as mentioned in Schedule, it is declared and agreed that
items listed in Annexure II (List 1) shall become payable up to Rs. 15,000/- in a policy period.
This Optional Cover is available for Sum Insured of 8 L & above.
Once this optional cover is opted and a claim has been admitted under the policy, You cannot
opt out of this optional cover.
SPECIFIC COVERAGES:
a) Artificial life maintenance, including life support machine use, where such treatment will not
result in recovery or restoration of normal state of Health under any circumstances. We cover
the expenses up to 10% of the Sum Insured and for a maximum of 15 days per policy period
for covered illness. This sub limit is applicable only for person who is declared to be in a
vegetative state as certified by the treating medical practitioner.
b) Puberty and Menopause related Disorders: Treatment for any symptoms, Illness,
complications arising due to physiological conditions associated with Puberty, Menopause
such as menopausal bleeding or flushing is covered only as Inpatient procedure after 24
months of continuous coverage. This cover will have a sub-limit of up to 25% of Sum Insured
per policy period.
c) Age Related Macular Degeneration (ARMD) is covered after 48 months of continuous
coverage only for Intravitreal Injections and anti - VEGF medication. This cover will have a sub-
limit of 10% of Sum Insured, maximum upto Rs. 75,000 per policy period.
UIN: NIAHLIP24123V032324 Page 6 of 24
NEW INDIA ASHA KIRAN POLICY
d) Genetic diseases or disorders are covered with a sub-limit of 25% of Sum Insured per policy
period with 48 months waiting periods.
Note: For the coverages defined in (a) to (d) above, waiting period's, if any, shall be applicable
afresh i.e. for both New and Existing Policyholders w.e.f 1
st
October 2020. Coverage for such
Illness or procedures shall only be available after completion of the said waiting periods.
e) Treatment of Mental Illness: The Company shall indemnify the Medical Expenses incurred
towards treatment of Mental Illness subject to the condition that Treatment shall be
undertaken at a Hospital categorized as Mental Health Establishment or at a Hospital with a
specific department for Mental Illness, under a Medical Practitioner qualified as Mental
Health Professional.
The following Mental Illnesses are covered after completion of 48 months of Continuous
Coverage with a sub-limit up to 25% of Sum Insured per policy period.
ICD Code
ICD Code Description
F01-F09
Mental disorders due to known physiological conditions
F10-F19
Mental and behavioral disorders due to psychoactive substance use
F20-F29
Schizophrenia, schizotypal, delusional, and other non-mood psychotic disorders
F60-F69
Disorders of adult personality and behavior
F70-F79
Intellectual disabilities
Exclusion: Any kind of Psychological counselling, cognitive/ family/ group/ behaviour/ palliative
therapy or psychotherapy shall not be covered.
COVERAGE FOR MODERN TREATMENTS or PROCEDURES: The following procedures will be
covered (wherever medically indicated) either as in patient or as part of day care treatment in
a hospital up to the limit specified against each procedure during the policy period.
Treatment or Procedure
Limit (Per Policy Period)
Uterine Artery Embolization and HIFU (High intensity
focused ultrasound)
Up to 20% of Sum Insured subject to
Maximum Rs. 1 Lakh
Balloon Sinuplasty.
Up to 20% of Sum Insured subject to
Maximum Rs. 1 Lakh
Deep Brain stimulation.
Up to 50% of Sum Insured subject to M
maximum Rs. 1.5 Lakh
Oral chemotherapy.
Up to 10% of Sum Insured subject to
Maximum Rs. 50,000.
Immunotherapy- Monoclonal Antibody to be given as
injection.
Up to 25% of Sum Insured subject to
Maximum Rs 1 Lakh.
Intravitreal injections.
Up to 10% of Sum Insured subject to
Maximum Rs.30,000.
Robotic surgeries.
Up to 50% of Sum Insured subject to
Maximum Rs. 2 Lakh.
Stereotactic radio surgeries.
Up to 50% of Sum Insured subject to
Maximum Rs. 1.5 Lakh.
UIN: NIAHLIP24123V032324 Page 7 of 24
NEW INDIA ASHA KIRAN POLICY
Bronchial Thermoplasty.
Up to 50% of Sum Insured subject to
Maximum Rs. 1.5 Lakh.
Vaporisation of the prostrate (Green laser treatment or
holmium laser treatment).
Up to 50% of Sum Insured subject to
Maximum Rs. 1.5 Lakh.
IONM - (Intra Operative Neuro Monitoring).
Up to 10% of Sum Insured subject to
Maximum Rs. 25,000.
Stem cell therapy: Hematopoietic stem cells for bone
marrow transplant for haematological conditions to be
covered.
Up to 50% of Sum Insured subject to
Maximum Rs. 1.5 Lakh.
SECTION II: PERSONAL ACCIDENT (APPLICABLE TO PROPOSER AND SPOUSE)
If the Proposer and/or Spouse shall sustain any bodily Injury resulting solely and directly from
Accident then We shall pay to dependent daughter(s) as specified in the schedule, the sum
hereinafter set forth that is to say:
If such Injury shall within twelve calendar months of its occurrence be the sole and direct cause of
Coverage
Compensation
Death of
Proposer or Spouse
100% of Sum Insured
Proposer and Spouse
200% of Sum Insured
Permanent Total Disablement of
Proposer or Spouse
100% of Sum Insured
Proposer and Spouse
200% of Sum Insured
Loss of both eyes / Loss of both limbs /
Loss of one limb and one eye of
Proposer or Spouse
100% of Sum Insured
Proposer and Spouse
200% of Sum Insured
Loss of one limb / one eye of
Proposer or Spouse
50% of Sum Insured
Proposer and Spouse
100% of Sum Insured
If the dependent daughter(s) specified in the schedule, is/are minor at the time of claim, then
the money will be deposited as fixed deposit in a Nationalized Bank, to be paid to daughter(s)
after attaining majority.
Note: The Company shall not be liable under this Policy for Compensation under more than
one of the sub-clauses, as mentioned above, in respect of same Injury or disablement.
In the event of unfortunate death of all the Insured Persons specified in the policy, no such
benefits shall be payable under this Section.
Any payment under this Clause would be in addition to the Sum Insured and shall not deplete
the Sum Insured.

UIN: NIAHLIP24123V032324 Page 8 of 24
NEW INDIA ASHA KIRAN POLICY
5. WHAT IS HOSPITAL CASH BENEFIT?
This policy provides for payment of Hospital Cash at the rate of 0.1% of Sum Insured per day of
Hospitalisation. This benefit will be given in every case of admissible claim and for each member. This
benefit is applicable only where Hospitalisation exceeds twenty four consecutive hours.
The total payment for Any One Illness shall not exceed 1% of the Sum Insured. This benefit shall be directly
given by TPA/underwriting office, as the case may be.
6. WHAT IS CRITICAL CARE BENEFIT?
If during the Period of Insurance any Insured Person discovers that he/she is suffering from any Critical
Illnesses as listed below and as defined under 2.8 of the Policy Clause, which results in a claim admissible
under this Policy, we will pay flat 10% of Sum Insured as additional benefit i.e. over and above the
admissible claim:
a Cancer of Specified severity
b First Heart attack of specified severity
c Open chest CABG
d Open Heart replacement or repair of Heart valves
e Coma of specified severity
f Kidney failure requiring regular dialysis
g Stroke resulting in permanent symptoms
h Major organ / bone marrow transplant
i Permanent paralysis of limbs
j Motor neurone disease with permanent symptoms
k Multiple sclerosis with persisting symptoms
Any payment under this clause would be in addition to the Sum Insured and shall not deplete the Sum
Insured. This benefit will be paid once in lifetime of any Insured Person. This benefit is not applicable for
those Insured Persons for whom it is a pre-existing disease.
7. IS PRE-ACCEPTANCE MEDICAL CHECK-UP REQUIRED?
Pre-acceptance test is required for all the members entering after the age of 50 for the first time. A person
also needs to undergo this pre-acceptance medical check-up if he has an adverse medical history. The cost
of this check-up will be borne by the proposer. But if the proposal is accepted, then 50% of the cost of this
check-up will be reimbursed to the proposer. List of Medical Tests required are as below.
CBC
Serum HDL
Blood Sugar Fasting & Post Prandial
Routine Urine Examination (RUE)
SGPT
Resting ECG
SGOT
X RAY Chest PA View
Serum Cholesterol
Physician Check Up
Serum Triglycerides
Eye Check Up For Cataract & Glaucoma

UIN: NIAHLIP24123V032324 Page 9 of 24
NEW INDIA ASHA KIRAN POLICY
8. DOES IT COVER ALL CASES OF HOSPITALISATION?
No claim will be payable under this Policy for the following:
STANDARD EXCLUSIONS
PRE-EXISTING DISEASES (Code- Excl01)
a. Expenses related to the treatment of a pre-existing Disease (PED) and its direct complications
shall be excluded until the expiry of 48 months of continuous coverage after the date of inception
of the first policy with us.
b. In case of enhancement of Sum Insured the exclusion shall apply afresh to the extent of Sum
Insured increase.
c. If the Insured Person is continuously covered without any break as defined under the portability
norms of the extant IRDAI (Health Insurance) Regulations then waiting period for the same would
be reduced to the extent of prior coverage.
d. Coverage under the policy after the expiry of 48 months for any pre-existing disease is subject to
the same being declared at the time of application and accepted by us.
SPECIFIC WAITING PERIOD (Code- Excl02)
a. Expenses related to the treatment of the following listed conditions, surgeries / treatments shall
be excluded until the expiry of Ninety Days / 24 / 48 months of continuous coverage, as may be
the case after the date of inception of the first policy with the insurer. This exclusion shall not be
applicable for claims arising due to an accident.
b. In case of enhancement of sum insured the exclusion shall apply afresh to the extent of sum
insured increase.
c. If any of the specified disease/procedure falls under the waiting period specified for preexisting
diseases, then the longer of the two waiting periods shall apply.
d. The waiting period for listed conditions shall apply even if contracted after the policy or declared
and accepted without a specific exclusion.
e. If the Insured Person is continuously covered without any break as defined under the applicable
norms on portability stipulated by IRDAI, then waiting period for the same would be reduced to
the extent of prior coverage.
i. 90 Days Waiting Period
1. Diabetes Mellitus
2. Hypertension
3. Cardiac Conditions
ii. 24 Months waiting period
1. All internal and external benign tumours, cysts, polyps of any kind, including benign breast
lumps

UIN: NIAHLIP24123V032324 Page 10 of 24
NEW INDIA ASHA KIRAN POLICY
2. Benign ear, nose, throat disorders
3. Benign prostate hypertrophy
4. Cataract and age related eye ailments
5. Gastric/ Duodenal Ulcer
6. Gout and Rheumatism
7. Hernia of all types
8. Hydrocele
9. Non Infective Arthritis
10. Piles, Fissures and Fistula in anus
11. Pilonidal sinus, Sinusitis and related disorders
12. Prolapse inter Vertebral Disc and Spinal Diseases unless arising from accident
13. Skin Disorders
14. Stone in Gall Bladder and Bile duct, excluding malignancy
15. Stones in Urinary system
16. Treatment for Menorrhagia/Fibromyoma, Myoma and Prolapsed uterus
17. Varicose Veins and Varicose Ulcers
18. Puberty and Menopause related Disorders
19. Internal Congenital Diseases
iii. 48 Months waiting period
1. Joint Replacement due to Degenerative Condition
2. Age-related Osteoarthritis & Osteoporosis
3. Treatment of mental illness
4. Age Related Macular Degeneration (ARMD)
5. Genetic diseases or disorders
6. External Congenital Diseases
FIRST THIRTY DAYS WAITING PERIOD (Code- Excl03)
a. Expenses related to the treatment of any illness within 30 days from the first policy
commencement date shall be excluded except claims arising due to an accident, provided the
same are covered.
b. This exclusion shall not, however, apply if the Insured Person has Continuous Coverage for more
than twelve months.
c. The within referred waiting period is made applicable to the enhanced sum insured in the event
of granting higher sum insured subsequently.
EXCLUSIONS
The Company shall not be liable to make any payment under the policy, in respect of any expenses
incurred in connection with or in respect of:
INVESTIGATION & EVALUATION (Code- Excl04)
a. Expenses related to any admission primarily for diagnostics and evaluation purposes.

UIN: NIAHLIP24123V032324 Page 11 of 24
NEW INDIA ASHA KIRAN POLICY
b. Any diagnostic expenses which are not related or not incidental to the current diagnosis and
treatment
REST CURE, REHABILITATION AND RESPITE CARE (Code- Excl05) Expenses related to any admission
primarily for enforced bed rest and not for receiving treatment. This also includes:
a. Custodial care either at home or in a nursing facility for personal care such as help with activities
of daily living such as bathing, dressing, moving around either by skilled nurses or assistant or
non-skilled persons.
b. Any services for people who are terminally ill to address physical, social, emotional and spiritual
needs.
OBESITY/ WEIGHT CONTROL (Code- Excl06) Expenses related to the surgical treatment of obesity that
does not fulfil all the below conditions:
a. Surgery to be conducted is upon the advice of the Doctor
b. The surgery/Procedure conducted should be supported by clinical protocols
c. The member has to be 18 years of age or older and
d. Body Mass Index (BMI);
1. greater than or equal to 40 or
2. greater than or equal to 35 in conjunction with any of the following severe comorbidities
following failure of less invasive methods of weight loss:
i. Obesity-related cardiomyopathy
ii. Coronary heart disease
iii. Severe Sleep Apnea iv. Uncontrolled Type2 Diabetes
CHANGE-OF-GENDER TREATMENTS (Code- Excl07)
Expenses related to any treatment, including surgical management, to change characteristics of the
body to those of the opposite sex.
COSMETIC OR PLASTIC SURGERY (Code- Excl08)
Expenses for cosmetic or plastic surgery or any treatment to change appearance unless for
reconstruction following an Accident, Burn(s) or Cancer or as part of medically necessary treatment to
remove a direct and immediate health risk to the insured. For this to be considered a medical necessity,
it must be certified by the attending Medical Practitioner.
HAZARDOUS OR ADVENTURE SPORTS (Code- Excl09)
Expenses related to any treatment necessitated due to participation as a professional in hazardous or
adventure sports, including but not limited to, para-jumping, rock climbing, mountaineering, rafting,
motor racing, horse racing or scuba diving, hand gliding, sky diving, deep-sea diving.
BREACH OF LAW (Code- Excl10)
Expenses for treatment directly arising from or consequent upon any Insured Person committing or
attempting to commit a breach of law with criminal intent.
EXCLUDED PROVIDERS (Code-Excl11)
Expenses incurred towards treatment in any hospital or by any Medical Practitioner or any other
provider specifically excluded by the Insurer and disclosed in its website / notified to the policyholders
are not admissible. However, in case of life-threatening situations or following an accident, expenses
up to the stage of stabilization are payable but not the complete claim.
Treatment for, Alcoholism, drug or substance abuse or any addictive condition and consequences
thereof. (Code- Excl12)

UIN: NIAHLIP24123V032324 Page 12 of 24
NEW INDIA ASHA KIRAN POLICY
Treatments received in health hydros, nature cure clinics, spas or similar establishments or private
beds registered as a nursing home attached to such establishments or where admission is arranged
wholly or partly for domestic reasons. (Code- Excl13)
Dietary supplements and substances that can be purchased without prescription, including but not
limited to Vitamins, minerals and organic substances unless prescribed by a medical practitioner as
part of hospitalization claim or day care procedure. (Code- Excl14)
REFRACTIVE ERROR (Code- Excl15)
Expenses related to the treatment for correction of eye sight due to refractive error less than
7.5 dioptres.
UNPROVEN TREATMENTS (Code- Excl16)
Expenses related to any unproven treatment, services and supplies for or in connection with any
treatment. Unproven treatments are treatments, procedures or supplies that lack significant medical
documentation to support their effectiveness.
STERILITY AND INFERTILITY (Code- Excl17)
Expenses related to sterility and infertility. This includes:
a. Any type of contraception, sterilization
b. Assisted Reproduction services including artificial insemination and advanced reproductive
technologies such as IVF, ZIFT, GIFT, ICSI
c. Gestational Surrogacy
d. Reversal of sterilization
MATERNITY EXPENSES (Code - Excl18)
a. Medical treatment expenses traceable to childbirth (including complicated deliveries and
caesarean sections incurred during hospitalization) except ectopic pregnancy;
b. Expenses towards miscarriage (unless due to an accident) and lawful medical termination of
pregnancy during the policy period.
SPECIFIC EXCLUSIONS
Acupressure, acupuncture, magnetic therapies.
Any expenses incurred on Domiciliary Hospitalization.
Service charges, Surcharges, Luxury Tax, Admission fees, Registration fees, Record Charges and
Telephone Charges levied by the Hospital.
Bodily Injury or Illness due to willful or deliberate exposure to danger (except in an attempt to save
human life), intentional self-inflicted Injury and attempted suicide.
Circumcision unless Medically Necessary or as may be necessitated due to an Accident.
Convalescence and General debility.
Cost of braces, equipment or external prosthetic devices, eyeglasses, Cost of spectacles and contact
lenses, hearing aids including cochlear implants.
External Medical / Non-medical equipment used for diagnosis and/or treatment including
CPAP/BIPAP, Oxygen Concentrator, Infusion pump , Ambulatory devices (walker, crutches, Collars,
Caps, Splints, Elasto crepe bandages, external orthopaedic pads) and sub cutaneous insulin pump,
Diabetic foot wear, Glucometer / Thermometer and equipment, which is subsequently used at home
and outlives the use and life of the Insured Person.
Naturopathy Treatment.
Nuclear, chemical or biological attack or weapons, contributed to, caused by, resulting from or from
any other cause or event contributing concurrently or in any other sequence to the loss, claim or
expense. For the purpose of this exclusion:

UIN: NIAHLIP24123V032324 Page 13 of 24
NEW INDIA ASHA KIRAN POLICY
a. Nuclear attack or weapons means the use of any nuclear weapon or device or waste or
combustion of nuclear fuel or the emission, discharge, dispersal, release or escape of fissile/
fusion material emitting a level of radioactivity capable of causing any Illness, incapacitating
disablement or death.
b. Chemical attack or weapons means the emission, discharge, dispersal, release or escape of any
solid, liquid or gaseous chemical compound which, when suitably distributed, is capable of
causing any Illness, incapacitating disablement or death.
c. Biological attack or weapons means the emission, discharge, dispersal, release or escape of any
pathogenic (disease producing) micro-organisms and/or biologically produced toxins (including
genetically modified organisms and chemically synthesized toxins) which are capable of causing
any Illness, incapacitating disablement or death.
Stem cell implantation/Surgery for other than those treatments mentioned in clause 3.14.12 of the
Policy Clause.
Treatments such as Rotational Field Quantum Magnetic Resonance (RFQMR), External Counter
Pulsation (ECP), Enhanced External Counter Pulsation (EECP), Hyperbaric Oxygen Therapy.
Treatment taken outside the geographical limits of India.
Vaccination and/or inoculation.
War (whether declared or not) and war like occurrence or invasion, acts of foreign enemies, hostilities,
civil war, rebellion, revolutions, insurrections, mutiny, military or usurped power, seizure, capture,
arrest, restraints and detainment of all kinds.
Payment or compensation in respect of death, Injury or disablements directly or indirectly arising out
of or contributed to or traceable to any disability already existing on the date of commencement of
this policy.
Procedures / treatments usually done in outpatient department are not payable under the Policy even
if converted as an in-patient in the Hospital for more than twenty-four consecutive hours.
Change of treatment from one system to another unless recommended by the consultant/
Hospital under which the treatment is taken.
9. WHAT IS A PRE EXISTING DISEASE?
The term Pre-existing condition/disease is defined in the Policy. It means any condition, ailment, Injury or
Illness
a. That is/are diagnosed by a physician within 48 months prior to the effective date of the Policy issued
by Us and its reinstatement or
b. For which medical advice or treatment was recommended by, or received from, a physician within 48
months prior to the effective date of the Policy or its reinstatement.
10. IS HOSPITALISATION ALWAYS NECESSARY TO GET A CLAIM?
Yes. Unless the Insured Person is Hospitalised for a condition warranting Hospitalisation, no claim is payable
under the Policy. The Policy does not cover outpatient treatments.
In case of Death Claim, Hospitalisation is not required but the death certificate, post mortem
report and police report is required.
UIN: NIAHLIP24123V032324 Page 14 of 24
NEW INDIA ASHA KIRAN POLICY
In case of Disability, Hospitalisation is not required but medical certificate certifying the
disablement and police report (if any) is required
11. HOW LONG DOES THE INSURED PERSON NEED TO BE HOSPITALISED?
The Policy pays only where the Hospitalisation is for more than twenty-four hours. But for certain
treatments specified in the Policy, period of stay at the Hospital could be less than twenty-four hours.
12. WHAT ARE THE DAY CARE TREATMENTS COVERED UNDER THIS POLICY?
Day Care Procedures shall be as per Annexure 1 of the Policy Clause.
13. WHAT DO I NEED TO DO IF ANYBODY COVERED IN THE POLICY NEEDS TO GET HOSPITALISED?
For Hospitalization Claim
Upon the happening of any event which may give rise to a claim under the policy, please immediately
intimate the TPA named in the schedule with all the details such as name of the Hospital, details of
treatment, patient name, policy number etc.
In case of emergency Hospitalisation, this information needs to be given to the TPA, within 24 hours from
the time of Hospitalisation.
For Personal Accident:
In case of death claim:
Nominee as specified in the policy schedule should immediately notify the policy issuing office
Submit the claim form along with death certificate, post mortem report, police report and original
policy.
In case of Injury claim:
Notify the policy issuing office immediately.
Submit Police report if any.
Submit claim form along with medical certificate certifying the disablement.
These are important conditions that you need to comply with.
14. WHAT ARE THE AMBULANCE CHARGES PAID UNDER THIS POLICY?
Company will pay ambulance charges up to 1% of SI or actual whichever is less. These charges are available
in case of emergency extraction from anywhere to Hospital or Hospital to Hospital.
15. IS PAYMENT AVAILABLE FOR EXPENSES INCURRED BEFORE HOSPITALISATION?
Yes. Medical Expenses incurred immediately before, but not exceeding thirty days, the Insured Person is
Hospitalised will be paid, provided that:
i. Such Medical Expenses are incurred for the same condition for which the Insured Person’s
Hospitalisation was required, and

UIN: NIAHLIP24123V032324 Page 15 of 24
NEW INDIA ASHA KIRAN POLICY
ii. The In-patient Hospitalisation claim for such Hospitalisation is admissible by Us.
16. IS PAYMENT AVAILABLE FOR EXPENSES INCURRED AFTER HOSPITALISATION?
Yes. Medical Expenses incurred immediately after, but not exceeding sixty days, the Insured Person is
discharged from the Hospital will be paid, provided that:
i. Such Medical Expenses are incurred for the same condition for which the Insured Person’s
Hospitalisation was required, and
ii. The In-patient Hospitalisation claim for such Hospitalisation is admissible by Us.
17. IS THERE A LIMIT TO WHAT THE COMPANY WILL PAY FOR HOSPITALISATION?
Yes. We will pay Hospitalisation expenses upto a limit, known as Sum Insured. In cases where the Insured
Person was Hospitalised more than once, the total of all amounts paid
a) for all cases of Hospitalisation,
b) expenses paid for medical expenses prior to Hospitalisation, and
c) expenses paid for medical expenses after discharge from Hospital Shall not exceed the Sum
Insured.
The Sum Insured under the policy is available for any or all the members covered for one or more claims
during the tenure of the policy.
For Personal accident, the coverage will be as described under Section II of Q.4
18. CAN I GET TREATED ANYWHERE IN INDIA?
The Policy covers treatment only in India. Even within India, if premium is paid for lower Zone and
treatment taken in higher Zone, our liability towards any claim will be 80% of admissible claim amount or
Sum Insured, whichever is less. Zone Classification is given below.
Illustration:
1) Insured XYZ, Sum Insured: Rs. 200000, Zone Selected: Zone III
Admissible Claim: Rs. 80000, Treatment taken in: Zone II
In such case Our liability will be 80% of the admissible claim amount i.e. Rs. 64000 (80% of Rs. 80000). Rest
of the amount will be borne by the Insured i.e. Rs. 16000.
2) Insured ABC, Sum Insured: Rs. 200000, Zone Selected: Zone II
Admissible Claim: Rs. 300000, Treatment taken in: Zone I
In such case, our liability will be 80% of admissible claim amount i.e. Rs. 240000 (80% of Rs. 300000). But
the claim amount cannot exceed the Sum Insured viz. Rs. 200000. Thus our total liability will be Rs. 200000.
UIN: NIAHLIP24123V032324 Page 16 of 24
NEW INDIA ASHA KIRAN POLICY
Note: Co-pay will not be applied on the Sum Insured, it is always applicable on the admissible claim
amount.
Zone- I
Greater Mumbai (includes Mira-Bhayandar, Thane, Navi Mumbai, Kalyan-Dombivli,
Ulhasnagar, Ambarnath, Badlapur) and State of Gujarat
Zone-II
Delhi NCR (includes Faridabad, Gurgaon, Mewat, Rohtak, Sonepat, Rewari, Jhajjhar,
Panipat and Palwal, Meerut, Ghaziabad, GautamBudha Nagar, Bulandshahr, and
Baghpat, Alwar and NCT of Delhi), Bangalore, Chennai, Hyderabad and
Secunderabad, Pune and Kolkata
Zone-III
Rest of India (other than those areas specified in Zone I and II)
The Cities mentioned below would include their Urban Agglomeration. The Insured Person can choose
the Zone at the time of proposal, and can also change it at the time of renewal. It is therefore in
your interest to choose the appropriate Zone and pay the necessary premium depending upon
your preference for coverage.
19. WHAT SUM INSURED SHOULD I CHOOSE?
You are free to choose any Sum Insured from Rs. 2, 3, 5, 8, 10, 12 and 15 Lakhs. The premium payable is
determined based on the following criteria:
a. The premium for the eldest member of the family. (Premium from Primary Member Premium
Table)
b. Premium for All additional members to be covered in this policy. (Premium from Additional
Member Premium Table)
c. Premium for the daughter(s) shall be 50% of her premium from Additional Member Premium
Table.
d. Sum Insured
e. Zone
You are free to choose any Sum Insured available as specified above. But it is in your own interest to choose
the Sum Insured which could satisfy your present as well as future needs.
20. HOW LONG IS THE POLICY VALID?
The Policy is valid during the Period of Insurance stated in the Schedule attached to the Policy. It is usually
valid for a period of one year from the date of beginning of insurance.
21. CAN THE POLICY BE RENEWED WHEN THE PRESENT POLICY EXPIRES?
Yes. You can and to get all Continuity benefits under the Policy, you should renew the Policy before the
expiry of the present policy. For instance, if Your Policy commences from 2nd October, 2021 date of expiry
is usually on 1st October, 2022. You should renew Your Policy by paying the Renewal Premium on or before
1st October 2022.

UIN: NIAHLIP24123V032324 Page 17 of 24
NEW INDIA ASHA KIRAN POLICY
The Company, with prior approval of lRDAl, may withdraw, revise or modify the terms of the policy
including the premium rates. The insured person shall be notified three months before the changes are
effected.
You can choose to migrate to any of our existing Policy, subject to Regulations of IRDAI (Protection of
Policyholders’ Interest) Regulations, 2017 and the Guidelines of IRDAI on Portability and Migration of
Health Insurance Policies, as amended from time to time.
Please note that:
i. The Company shall endeavor to give notice for renewal. However, the Company is not under
obligation to give any notice for renewal.
ii. Renewal shall not be denied on the ground that the insured person had made a claim or claims in
the preceding policy years.
iii. Request for renewal along with requisite premium shall be received by the Company before the end
of the policy period.
iv. At the end of the policy period, the policy shall terminate and can be renewed within the Grace
Period of 30 days to maintain continuity of benefits without break in policy. Coverage is not available
during the Grace Period.
v. No loading shall apply on renewals based on individual claims experience.
22. WHAT IS CONTINUITY BENEFIT?
There are certain treatments which are payable only after the Insured Person is continuously covered for
a specified period. For example, Cataract is covered only after twenty-four months of Continuous Coverage.
If an Insured took a Policy in October, 2019, does not renew it on time and takes a Policy only in December
2020, and renewed it on time in December 2021, any claim for Cataract would not become payable,
because the Insured Person was not continuously covered for twenty-four months. If, he had renewed the
Policy in time in October 2020 and then in October 2021, then he would have been continuously covered
for twenty-four months and therefore his claim for Cataract in the Policy beginning from October 2021
would be payable. Therefore, you should always ensure that you pay your renewal Premium before Your
Policy expires.
23. IS THERE ANY GRACE PERIOD FOR RENEWAL OF THE POLICY?
Yes. If Your Policy is renewed within thirty days of the expiry of the previous Policy, then the Continuity
Benefits would not be affected. But even if You renew Your Policy within thirty days of expiry of previous
Policy, any Illness contracted or Injury sustained or Hospitalisation commencing during the break in
insurance is not covered. Therefore, it is in your own interest to see that you renew the Policy before it
expires.
24. CAN THE SUM INSURED BE INCREASED AT THE TIME OF RENEWAL?
Yes. You may seek enhancement of Sum Insured in writing before payment of premium for renewal, which
may be granted at Our discretion. Before granting such request for enhancement of Sum Insured, We have
the right to have You examined by a Medical Practitioner authorized by Us or the TPA (50% of Medical
examination cost will be reimbursed to the Insured Person). Our consent for enhancement of Sum Insured
is dependent on the recommendation of the Medical Practitioner.
Enhancement of Sum Insured shall be allowed based on the following table:
Age<=50 years
Enhancement up to Sum Insured of 15 lakhs without Medical Examination.
Age 51-60 Years
Enhancement by two slabs without Medical Examination
Age 51-60 Years
Enhancement up to 15 Lakhs with Medical Examination
Age 61-65 Years
Enhancement by one slab with Medical Examination

UIN: NIAHLIP24123V032324 Page 18 of 24
NEW INDIA ASHA KIRAN POLICY
Enhancement of Sum Insured will not be considered for:
1) Insured Persons over 65 years of age.
2) Insured Person who had undergone Hospitalization in the preceding two years.
3) Insured Persons suffering from one or more of the following Illnesses/Conditions:
i Any chronic Illness/ Ailment
ii Any recurring Illness/ Ailment
iii Any Critical Illness
In respect of any increase in Sum Insured, exclusion 4.1, 4.2, 4.3 would apply to the additional Sum Insured
from the date of such increase.
25. IS THERE AN AGE LIMIT UPTO WHICH THE POLICY WOULD BE RENEWED?
No. Your Policy can be renewed, as long as you pay the Renewal Premium before the date of expiry of the
Policy. There is an age limit for taking a fresh Policy, but there is no age limit for renewal.
Children between 18 years to 25 years can be continue to be covered in the Policy provided they are
financially dependent on the parents and one or both parents are covered simultaneously. On attaining the
age of 18 years or ceasing to be financially dependent on the parents, they can, on renewal take a separate
Policy. In such an event the benefits on Continuous Coverage can be ported to the new Policy. The upper
age limit will not apply to a mentally challenged children and an unmarried dependent daughter(s).
If you do not renew Your Policy before the date of expiry or within thirty days of the date of expiry, the
Policy may not be renewed, and only a fresh Policy could be issued, subject to our underwriting rules. In
such cases, it is possible that a fresh Policy could not be issued by us. It is therefore in your interest to
ensure that Your Policy is renewed before expiry.
26. CAN THE INSURANCE COMPANY REFUSE TO RENEW THE POLICY?
We may refuse to renew the Policy only on rare occasions such as fraud, misrepresentation or non-
disclosure of material facts or non-cooperation being committed by You or any one acting on Your behalf
in obtaining insurance or subsequently in relation thereto. If we discontinue selling this Policy, it might not
be possible to renew this Policy on the same terms and conditions. In such a case you shall, however, have
the option for renewal under any similar Policy being issued by the Company, provided the benefits payable
shall be subject to the terms contained in such other Policy.
27. CAN I MAKE A CLAIM IMMEDIATELY AFTER TAKING A POLICY?
Claims for Illnesses cannot be made during the first thirty days of a fresh Insurance policy. However, claims
for Hospitalisation due to accidents occurring even during the first thirty days are payable. There are certain
treatments where the waiting period is 90 days, two years or four years.
28. WHAT IS THIRD PARTY ADMINISTRATOR (TPA)?
Third Party Administrator (TPA) is a service provider to facilitate service to you for providing Cashless facility
for all Hospitalisation that come under the scope of the policy. The TPA also settles reimbursement claims
within the scope of the Policy.
29. WHAT IS CASHLESS HOSPITALISATION?
Cashless Hospitalisation is service provided by the TPA on Our behalf whereby you are not required to
settle the Hospitalisation expenses at the time of discharge from Hospital. The settlement is done directly
by the TPA on Our behalf. However, those expenses which are not admissible under the Policy would not
be paid and you would have to pay such inadmissible expenses to the Hospital. Cashless facility is available
only in Networked Hospitals. Prior approval is required from the TPA before the patient is admitted into
the Networked Hospital. You may visit our Website at http://newindia.co.in/listofhospitals.aspx. The list of

UIN: NIAHLIP24123V032324 Page 19 of 24
NEW INDIA ASHA KIRAN POLICY
Networked Hospitals can also be obtained from the TPA or from their website. You will have full freedom
to choose the hospitals from the Networked Hospitals and avail Cashless facility on production of proof of
Insurance and Your identity, subject to the claim being admissible. The TPA might not agree to provide
Cashless facility at a Hospital which is not a Network Hospital. In such cases you may avail treatment at any
Hospital of Your choice and seek reimbursement of the claim subject to the terms and conditions of the
Policy. In cases where the admissibility of the claim could not be determined with the available documents,
even if the treatment is at a Network Hospital, the TPA may refuse to provide Cashless facility. Such refusal
may not necessarily mean denial of the claim. You may seek reimbursement of the expenses incurred by
producing all relevant documents and the TPA may pay the claim, if it is admissible under the terms and
conditions of the Policy.
30. CAN I CHANGE HOSPITALS DURING THE COURSE OF MY TREATMENT?
Yes, it is possible to shift to another hospital for reasons of requirement of better medical procedure.
However, this will be evaluated by Us / TPA on the merits of the case and as per policy terms and conditions.
31. HOW TO GET REIMBURSEMENTS IN CASE OF TREATMENT IN NON- NETWORK HOSPITALS OR DENIAL
OF CASHLESS FACILITY?
In case of treatment in a non-Network Hospital, TPA will reimburse You the amount of bills subject to the
conditions of the Policy. You must ensure that the Hospital where treatment is taken fulfills the conditions
of definition of Hospital in the Policy. Within twenty-four hours of Hospitalisation the TPA should be
intimated.
32. HOW TO GET REIMBURSEMENT FOR PRE AND POST HOSPITALISATION EXPENSES?
The Policy allows reimbursement of medical expenses incurred before and after admissible Hospitalisation
up to a certain number of days. For reimbursement, send all bills in original with supporting documents
along with a copy of the discharge summary and a copy of the authorization letter to his/her
TPA/underwriting office, whichever applicable. The bills must be sent to the TPA/underwriting office within
15 days from the date of completion of treatment. You must also provide the TPA/underwriting office with
additional information and assistance as may be required by the Company/TPA in dealing with the claim.
33. WILL THE ENTIRE AMOUNT OF THE CLAIMED EXPENSES BE PAID?
The entire amount of the claim is payable, if it is within the Sum Insured and is related with the
Hospitalisation as per Policy conditions and is supported by proper documents, except the expenses which
are excluded.
Personal Accident claims will be paid as mentioned Point 5 –Section II, without any deductions.
Hospitalisation cover is independent of Personal Accident cover. Upon happening of accident if the Insured
Person is Hospitalised, Hospitalisation will be paid in addition to compensation being paid under Personal
Accident coverage.
34. CAN ANY CLAIM BE REJECTED OR REFUSED?
Yes. A claim, which is not covered under the Policy conditions, can be rejected. Claims may also be rejected
in the event of misrepresentation, misdescription or nondisclosure of any material fact/particular. ln case
of any grievance the insured person may contact the company through
Website: https://www.newindia.co.in/portal/readMore/Grievances
Toll free: 1800-209-1415
E-mail, Fax and Courier: As mentioned in the above address
Senior Citizens may write to seniorcitizencare.ho@newindia.co.in
lnsured person may also approach the grievance cell at any of the company's branches with the details of
grievance.

UIN: NIAHLIP24123V032324 Page 20 of 24
NEW INDIA ASHA KIRAN POLICY
lf lnsured person is not satisfied with the redressal of grievance through one of the above methods, insured
person may contact the grievance officer at https://www.newindia.co.in/portal/readMore/Grievances For
updated details of grievance officer, kindly refer the link
https://www.newindia.co.in/portal/readMore/Grievances
lf lnsured person is not satisfied with the redressal of grievance through above methods, the insured person
may also approach the office of lnsurance Ombudsman of the respective area/region for redressal of
grievance as per lnsurance Ombudsman Rules 2017. Please refer to Annexure III of the Policy Clause.
Grievance may also be lodged at IRDAI lntegrated Grievance Management System - https://igms.
irdai.gov.in
35. CAN I CANCEL THE POLICY?
The policyholder may cancel this policy by giving 15 days written notice and in such an event, the Company
shall refund premium for the unexpired policy period at Our short period rate detailed below.
Period On Risk
Rate of Premium To Be Charged
(Retained By The Insurer)
Up to one month
1/4th of the annual rate
Up to three months
1/2 of the annual rate
Up to six months
3/4th of the annual rate
Exceeding six months
Full annual rate
In the event of death of insured in the middle of policy year/during the course of policy period, the premium
for the unexpired policy period shall be refunded proportionately.
Notwithstanding anything contained herein or otherwise, no refunds of premium shall be made in respect
of Cancellation where, any claim has been admitted or has been lodged or any benefit has been availed by
the insured person under the policy.
The Company may cancel the policy at any time on grounds of misrepresentation non-disclosure of material
facts, fraud by the insured person by giving 15 days' written notice. There would be no refund of premium
on cancellation on grounds of misrepresentation, non-disclosure of material facts or fraud.
36. WHAT IS FREE LOOK PERIOD?
The Free Look Period shall be applicable on new individual health insurance policies and not on renewals
or at the time of porting/migrating the policy.
The insured person shall be allowed free look period of fifteen days from date of receipt of the policy
document to review the terms and conditions of the policy, and to return the same if not acceptable.
lf the insured has not made any claim during the Free Look Period, the insured shall be entitled to
i. a refund of the premium paid less any expenses incurred by the Company on medical examination
of the insured person and the stamp duty charges or
ii. where the risk has already commenced and the option of return of the policy is exercised by the
insured person, a deduction towards the proportionate risk premium for period of cover or
iii. Where only a part of the insurance coverage has commenced, such proportionate premium
commensurate with the insurance coverage during such period;
37. IS THERE ANY BENEFIT UNDER THE INCOME TAX ACT FOR THE PREMIUM PAID FOR THIS INSURANCE?
Yes. Payments made for health insurance in any mode other than cash are eligible for deduction from
taxable income as per Section 80 D of the Income Tax Act, 1961. For details, please refer to the relevant
Section of the Income Tax Act.

UIN: NIAHLIP24123V032324 Page 21 of 24
NEW INDIA ASHA KIRAN POLICY
38. IF THE CLAIM EVENT FALLS WITHIN TWO POLICY PERIODS, HOW MUCH WILL BE PAID?
If the claim event falls within two policy periods, the claims shall be paid taking into consideration the
available Sum Insured of the expiring Policy only. Sum Insured of the Renewed Policy will not be available
for the Hospitalisation (including Pre & Post Hospitalisation Expenses), which has commenced in the
expiring Policy. Claim shall be settled on per event basis.
39. WHAT WILL HAPPEN TO THE POLICY WHEN THE DAUGHTER/S BECOMES FINANCIALLY DEPENDENT OR
A BOY CHILD IS BORN AFTER TAKING THE POLICY?
The Company shall offer an option to migrate to suitable Health Insurance policy once the Daughter/s
become financially independent or a Boy child is born after taking the policy.
UIN: NIAHLIP24123V032324 Page 22 of 24
NEW INDIA ASHA KIRAN POLICY
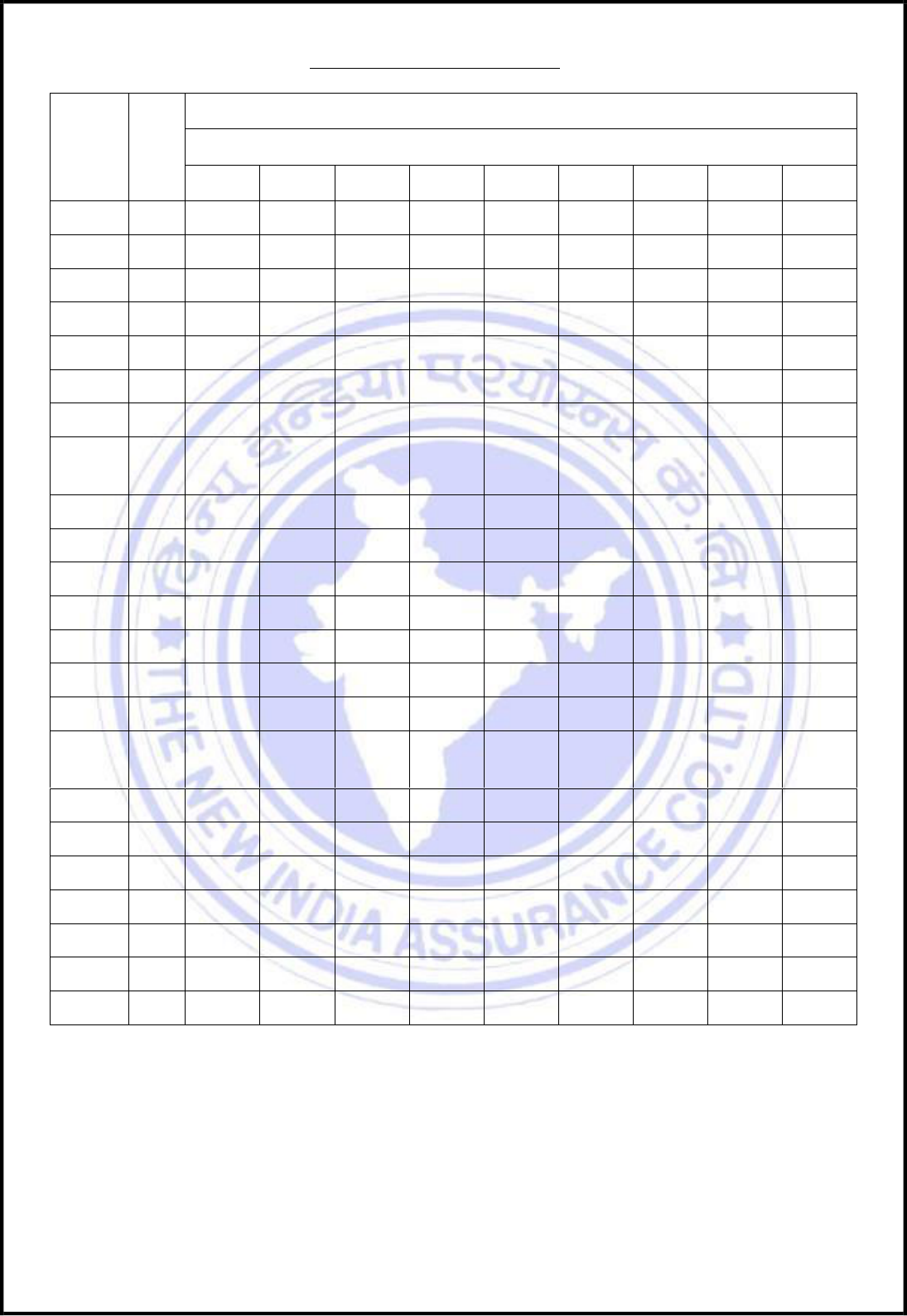
New India Asha Kiran Policy - Premium Chart (Excluding GST)
Sum
Insured
Zone
PRIMARY MEMBER Premiums applicable at different ages
(Rs. per annum excluding GST)
0-20 Y
21-30 Y
30-35 Y
36-40 Y
41-45 Y
46-50 Y
51-55 Y
56-60 Y
61-65 Y
2,00,000
I
2,930
3,986
4,742
5,813
7,545
9,215
12,869
15,750
26,555
3,00,000
I
4,087
5,396
6,086
7,424
9,643
11,775
17,111
20,903
35,339
5,00,000
I
5,829
7,917
8,914
10,907
12,667
15,479
23,287
28,474
48,348
8,00,000
I
7,157
9,715
10,950
13,394
15,562
19,001
28,590
35,507
59,359
10,00,000
I
8,170
11,096
12,493
15,286
17,753
21,694
32,637
39,645
67,316
12,00,000
I
8,882
12,063
13,582
16,618
19,300
23,585
35,481
43,040
73,082
15,00,000
I
10,069
13,675
15,397
18,840
21,880
26,737
40,223
48,705
82,700
Sum
Insured
Zone
0-20 Y
21-30 Y
30-35 Y
36-40 Y
41-45 Y
46-50 Y
51-55 Y
56-60 Y
61-65 Y
2,00,000
II
2,663
3,623
4,316
5,277
6,852
8,379
11,703
14,318
24,146
3,00,000
II
3,720
4,910
5,527
6,748
8,761
10,702
15,553
19,008
32,120
5,00,000
II
5,296
7,194
8,108
9,910
11,521
14,074
21,172
25,880
43,953
8,00,000
II
6,502
8,833
9,954
12,172
14,150
17,275
25,994
32,281
53,966
10,00,000
II
7,423
10,083
11,364
13,889
16,146
19,725
29,673
36,034
61,196
12,00,000
II
8,069
10,961
12,354
15,099
17,553
21,443
32,258
39,120
66,438
15,00,000
II
9,148
12,426
14,005
17,117
19,899
24,310
36,570
44,269
75,182
Sum
Insured
Zone
0-20 Y
21-30 Y
30-35 Y
36-40 Y
41-45 Y
46-50 Y
51-55 Y
56-60 Y
61-65 Y
2,00,000
III
2,394
3,261
3,891
4,757
6,174
7,545
10,538
12,884
21,735
3,00,000
III
3,352
4,425
4,969
6,072
7,879
9,629
13,994
17,111
28,916
5,00,000
III
4,765
6,470
7,303
8,914
10,374
12,667
19,055
23,287
39,558
8,00,000
III
5,846
7,951
8,959
10,962
12,739
15,548
23,399
29,056
48,574
10,00,000
III
6,678
9,068
10,236
12,493
14,539
17,753
26,707
32,423
55,077
12,00,000
III
7,259
9,858
11,128
13,582
15,806
19,300
29,034
35,200
59,794
15,00,000
III
8,230
11,176
12,615
15,397
17,919
21,880
32,914
39,833
67,664
UIN: NIAHLIP24123V032324 Page 23 of 24
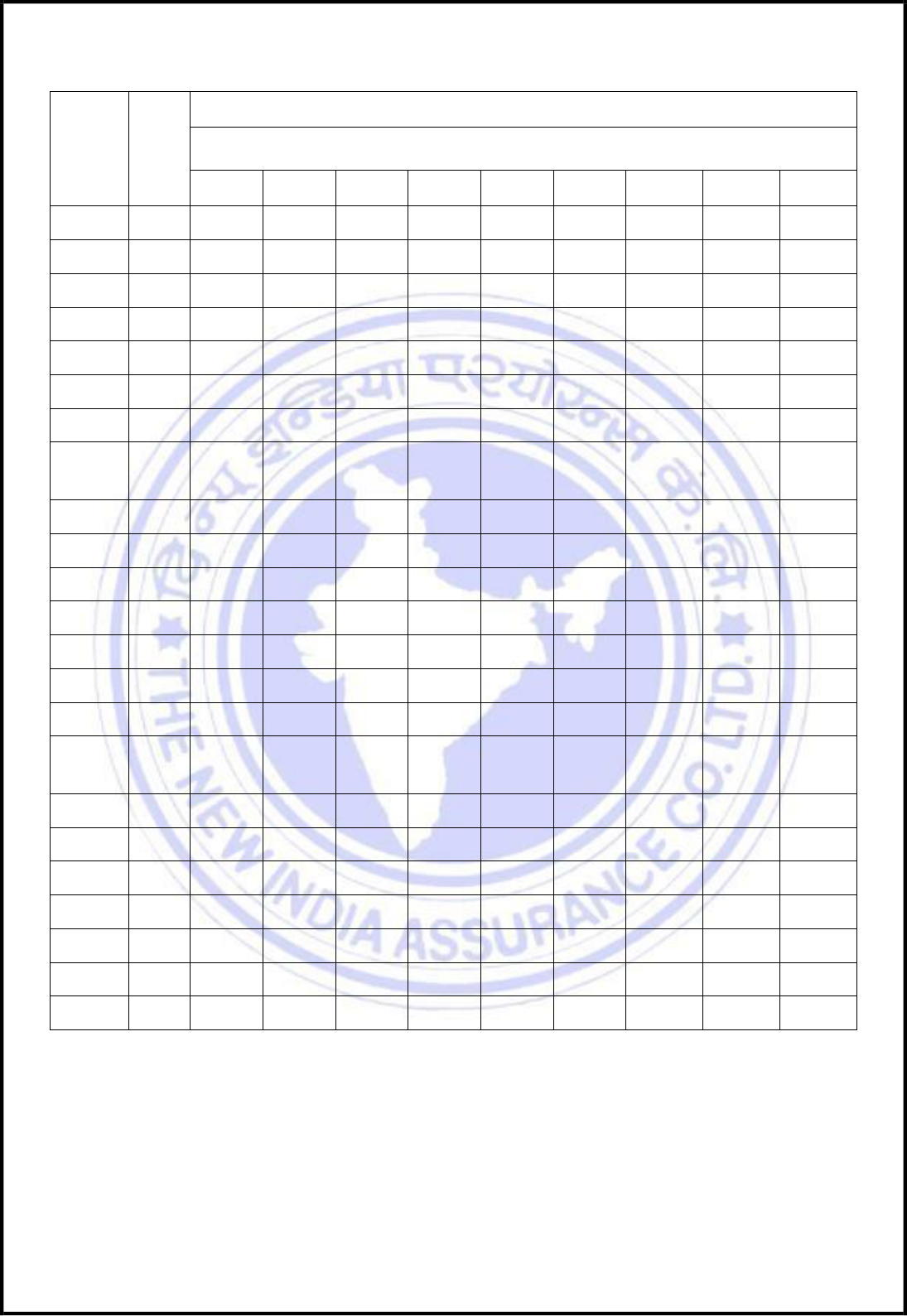
NEW INDIA ASHA KIRAN POLICY
Sum
Insured
Zone
ADDITIONAL MEMBER Premiums applicable at different ages
(Rs. per annum excluding GST)
0-20 Y
21-30 Y
30-35 Y
36-40 Y
41-45 Y
46-50 Y
51-55 Y
56-60 Y
61-65 Y
2,00,000
I
395
567
804
977
1,733
2,111
4,473
5,466
17,262
3,00,000
I
545
764
1,000
1,235
2,220
2,720
5,925
7,248
22,947
5,00,000
I
779
1,134
1,489
1,816
2,908
3,563
8,068
9,870
31,409
8,00,000
I
958
1,386
1,828
2,231
3,578
4,373
9,892
12,109
38,556
10,00,000
I
1,091
1,589
2,086
2,545
4,076
4,994
11,307
13,742
43,732
12,00,000
I
1,186
1,727
2,268
2,767
4,431
5,429
12,292
14,919
47,477
15,00,000
I
1,345
1,958
2,571
3,137
5,023
6,155
13,935
16,882
53,726
Sum
Insured
Zone
0-20 Y
21-30 Y
30-35 Y
36-40 Y
41-45 Y
46-50 Y
51-55 Y
56-60 Y
61-65 Y
2,00,000
II
363
521
725
882
1,575
1,922
4,064
4,962
15,687
3,00,000
II
500
692
911
1,117
2,015
2,470
5,380
6,586
20,860
5,00,000
II
710
1,024
1,352
1,652
2,648
3,236
7,331
8,969
28,556
8,00,000
II
870
1,260
1,663
2,029
3,251
3,970
8,996
11,012
35,053
10,00,000
II
995
1,436
1,895
2,316
3,711
4,535
10,274
12,487
39,759
12,00,000
II
1,081
1,561
2,060
2,518
4,035
4,930
11,169
13,557
43,164
15,00,000
II
1,226
1,769
2,335
2,854
4,574
5,589
12,662
15,341
48,845
Sum
Insured
Zone
0-20 Y
21-30 Y
30-35 Y
36-40 Y
41-45 Y
46-50 Y
51-55 Y
56-60 Y
61-65 Y
2,00,000
III
332
473
647
788
1,418
1,733
3,654
4,473
14,112
3,00,000
III
456
617
823
1,000
1,809
2,220
4,837
5,925
18,773
5,00,000
III
642
928
1,216
1,489
2,389
2,908
6,594
8,068
25,704
8,00,000
III
781
1,134
1,500
1,828
2,923
3,578
8,102
9,917
31,550
10,00,000
III
900
1,301
1,704
2,086
3,349
4,076
9,241
11,233
35,787
12,00,000
III
978
1,414
1,852
2,268
3,641
4,431
10,046
12,195
38,853
15,00,000
III
1,109
1,603
2,100
2,571
4,127
5,023
11,389
13,800
43,966
Premium will increase by 2% for every year after the age of 65 years for both Primary and Additional
members.
UIN: NIAHLIP24123V032324 Page 24 of 24
NEW INDIA ASHA KIRAN POLICY
Optional Covers – Per Member Premium (Excluding GST)
Sum Insured
(Rs.)
OPTIONAL COVER I : NO PROPORTIONATE DEDUCTION
<35
36-45
46-50
51-55
56-60
61-65
>65
2,00,000
1,418
1,506
2,483
3,741
4,852
6,419
9,201
3,00,000
980
1,040
1,715
2,584
3,351
4,434
6,355
5,00,000
770
817
1,348
2,031
2,634
3,485
4,995
8,00,000
646
686
1,131
1,704
2,210
2,924
4,191
10,00,000
662
703
1,159
1,747
2,265
2,997
4,296
12,00,000
644
684
1,127
1,699
2,203
2,915
4,178
15,00,000
458
487
802
1,209
1,568
2,075
2,974
OPTIONAL COVER II : MATERNITY EXPENSES BENEFIT
SI
5,00,000
8,00,000
10,00,000
12,00,000
15,00,000
(Rs.)
5,000
8,000
10,000
12,000
15,000
Sum Insured
(Rs.)
OPTIONAL COVER III : REVISION IN LIMIT OF CATARACT
<50
51-55
56-60
61-65
>65
8,00,000
444
1,049
2,269
3,645
3,893
10,00,000
555
1,311
2,836
4,556
4,866
12,00,000
666
1,573
3,404
5,467
5,839
15,00,000
832
1,967
4,255
6,834
7,299
Optional Cover IV: For Non-Medical Items (Consumables): This optional cover is for covering medical consumables (Non-Payable items).
It is applicable for Sum Insured of 8 L & above, and is payable up to a maximum of Rs. 15,000 per policy period. The premium charged for
this add on cover will be rated Rs 1500/- per member.
